An interview with Joanna G. Katzman, MD, MSPH, Professor, UNM School of Medicine; Director, UNM Pain Center; Director, ECHO Institute, Pain, Substance Use and Public Health Programs

Joanna G. Katzman, MD, MSPH
The University of New Mexico ( UNM) Pain Center was formed in 2011 and is one of the largest interdisciplinary pain programs in the southwest, and perhaps even in the US. At the UNM Pain Center, the clinicians providing care to patients suffering from chronic pain are an extremely diverse group. The clinicians include: anesthesiologists and physiatrists, with Pain Fellowship training, neurologist with training in neurorehabilitation and headache, family and community medicine physicians with training in myofascial pain, along with mental health clinicians, both psychology, and addiction psychiatry. The UNM Pain Center also has two advanced practice providers, two pharmacist clinicians, and two physical therapists. Patients are referred to the Pain Center by their primary care provider from throughout New Mexico as well as surrounding states. Approximately nine thousand patients visits are documented each year.
Every other week, the UNM Pain Center clinicians and staff meet for almost two hours for an interdisciplinary team meeting, where most new and many complex patients are discussed. In addition, the UNM Pain Center is the home to many clinical rotations, both for medical and physician assistant students as well as residents from many disciplines, including family practice, internal medicine, anesthesia, and pharmacy. The ACGME Pain Fellowship has four fellows each year, and Palliative Care Fellows also rotate every year for three months.
What has been the greatest challenge in combining the mix of providers and disciplines that are on your team?
The biggest challenge in bringing many disciplines together in one space to work closely in support of caring for patients with high impact pain- has been understanding how to share a common language around each clinicians’ discipline. In addition, it is vital to have all members of the team (from doctors to medical assistants) feel equally as valued as each other. For example, our patients may be in treatment with the physical therapist, the psychologist and one of the physicians. The patient also meets with the medical assistant and nurse at each visit too. The relationship between these clinicians is dependent on how well the patient does, because there is so much communication needed behind the scenes. Over the years of working closely together, we have developed much trust and respect for each other as colleagues who each bring a unique but equally vital importance to the team.
 Describe the relationship that your clinic has with primary care.
Describe the relationship that your clinic has with primary care.
The UNM Pain Center only accepts referrals from Primary Care clinicians. These clinicians practice in all 35 counties in New Mexico, and may also be located even at our UNM Health Sciences Center primary care clinics. Because we are a consultation and treatment center, our goal is to diagnose, and treat the patient with an interdisciplinary approach. But, once the patient is stabilized, we transfer care back to their primary care clinician with a thorough letter explaining their care plan. We don’t accept patients from other specialists in order to prioritize primary care referrals. In addition, we cannot see patients chronically, or we will not have the capacity to see new patients in our system.
 Does your clinic impact patients in your facility (or region) that are never actually seen in your clinic?
Does your clinic impact patients in your facility (or region) that are never actually seen in your clinic?
Yes, because our clinic addresses comprehensive pain management and has the capacity to serve thousands of patients each year, there is additional capacity in other clinics, urgent cares, emergency rooms, etc. for patients with chronic pain symptoms. Additionally, our pain center clinicians educate the region’s primary care clinicians and so they make more informed choices with their patient panel regarding pain treatment and opioid prescribing.
Because the UNM Pain Center manages patients from throughout New Mexico, southern Colorado, Eastern Arizona and the Navajo Nation,
 What do you think is important for key stakeholders (e.g., payors, providers, patients) to understand about ECHO for pain management?
What do you think is important for key stakeholders (e.g., payors, providers, patients) to understand about ECHO for pain management?
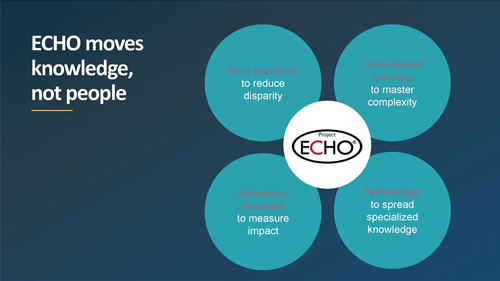
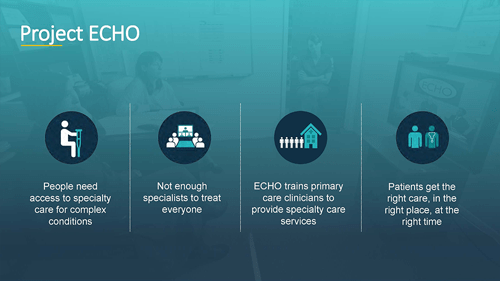
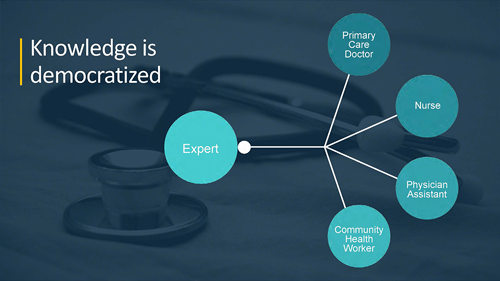
Project ECHO is a virtual telementoring program whereby subject matter experts at the “hub” provide case-based learning and evidence guided material to “spoke” clinicians in rural and urban underserved communities where there might not be readily available specialists. Clinicians earn one-hour of no-cost CME for every hour they join the ECHO network for a session. Project ECHO is now available in all 50 states and for over 70 different medical conditions. Because clinicians present real, de-identified cases at every ECHO session, these ECHO sessions have proven very beneficial for many clinicians interested in a best practices, quality approach to patient care. For busy clinicians, where their time is limited, they rarely have no more than one hour to spend on an ECHO session each week. There has been many conversations at the Federal level about novel ways to reimburse and/or account (RVU) clinicians for their time. And, although no patients are part of the ECHO network, patients are usually informed that their clinician may present their case to the ECHO network. Not surprisingly, most patients are delighted at the idea of a case conference devoted to their medical management.
 How does ECHO support the utilization of non-pharmacological therapies for pain for people in rural areas?
How does ECHO support the utilization of non-pharmacological therapies for pain for people in rural areas?
ECHO is extremely supportive of a multimodal approach to pain management. Much of our year-long didactic curriculum is focused on non-pharmacological approaches to chronic pain management. This includes: physical therapy, chiropractic treatment, acupuncture, massage, trigger point injections and dry needling, yoga and nutrition consultations. Because the ECHO sessions use Zoom as their platform, we are able to showcase many of these integrative approaches to pain management during an ECHO Pain session. These “hands-on” sessions are very popular among spoke clinicians and are requested year after year.
How has COVID19 impacted your clinic’s mission.
COVID-19 has impacted our UNM Pain Center’s mission insofar as to have more patients connect to our clinicians via Zoom instead of in-person. Our mission still remains the same. In fact, we are even more focused on bringing in new patients into our clinic more quickly as we realize that patients are isolated and may have a very difficult time accessing medical care. We definitely do not want their chronic pain to worsen while they are waiting to be seen. Additionally, we are acutely aware of the tremendous health care access disparities based on race and color- illuminated by the COVID-19 pandemic. This is something that makes healthcare difficult for chronic pain and substance use disorder even without the pandemic. Our clinic is attempting to remain focused on these disparities and to treat all people with equality.
How can interested stakeholders learn more about ECHO trainings you can provide, or what else do we need to know about ECHO as a resource that may not be currently widely known?
Please go to our Project ECHO Institute website to learn all about our programs here at the ECHO Institute in Albuquerque, New Mexico, as well as where the 240 hubs are located throughout the globe. Almost all ECHO sessions are open free of charge to all clinicians wherever you might live. On the ECHO Institute website, you can also learn all about upcoming trainings to launch your own ECHO!
Contact your local ECHO Hub to understand what programs they are offering.

Trackbacks/Pingbacks