
People with Pain, Payers, Clinicians, and Industry Discuss CMS Pain Codes + Scaling Transdisciplinary Pain Care
Webinar Date: December 7, 12:00-2:00 PM ET
On behalf of the Alliance to Advance Comprehensive Integrative Pain Management and the US Pain Foundation, we invite you to join this lively and constructive discussion about the intersection of payer policies and value-based care delivery for high-impact pain.
Register now for this no-cost webinar, Exploring Equitable, Scalable, Value-Based Pain Care Delivery, and share this survey with your networks to help gather feedback before the program.
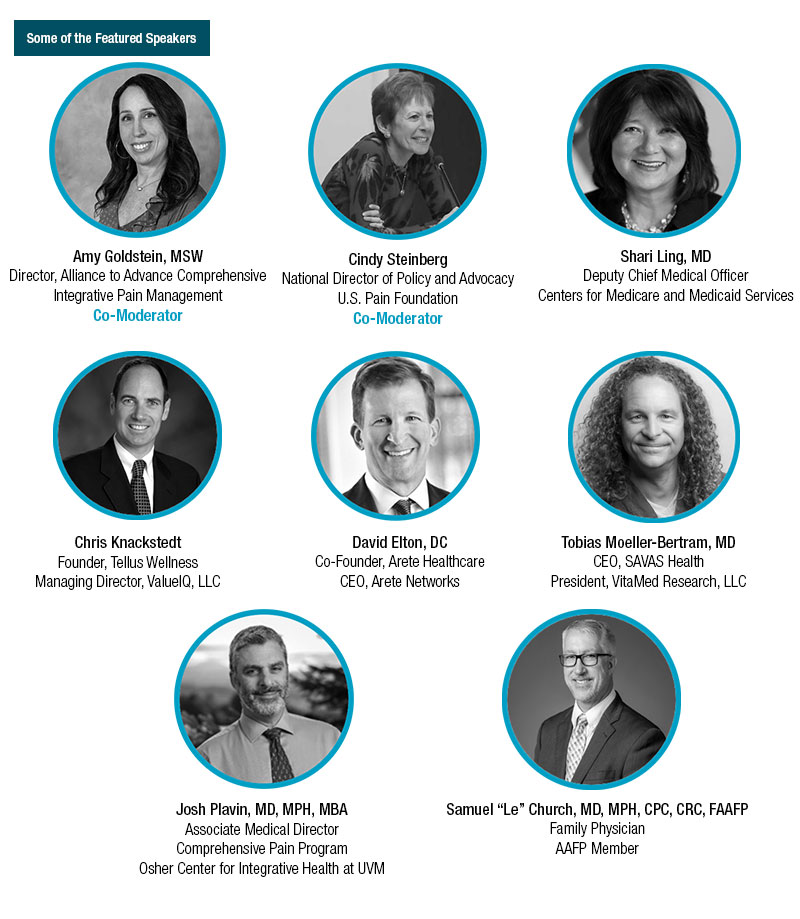
In light of CMS’ laudable goal for Medicare and Medicaid beneficiaries to be in value-based care relationships by 2030, we will take a deeper dive to explore the real-world impact of this goal and the paths toward successful implementation. This program will look into the most recent pain management codes released by CMS in January 2023 and how these are playing out in various clinical settings. Further, our esteemed panelists (see their bios) each bring a unique perspective and practical expertise to the conversation with an understanding of the nuances of how payer policies impact clinical—and scalable—implementation of pain care policy.
Participants in this free webinar will learn about:
- CMS efforts to advance value-based care, including the new CMS pain codes – what these are, what they mean, and how the first year since their release is going.
- Public and private sector innovation advancing access to transdisciplinary pain care for people who are underserved.
- Value-based care innovation that offers a network of chiropractors, acupuncturists, nutritionists, massage therapists, health coaches, and naturopaths.
- An example of family practice in rural Georgia and how the CMS codes impact value-based care delivery.
Whether or not you can attend the webinar, your feedback is crucial to webinar development, so please take a few minutes to complete this survey and/or share it with your networks.
National Updates
American Psychological Association Accepting Public Comment on Draft Guidelines for Chronic Musculoskeletal Pain in Adults
 The American Psychological Association (APA) is currently accepting public comments on its Draft APA Clinical Practice Guideline for the Treatment of Chronic Musculoskeletal Pain in Adults. The guideline focuses on recommendations for psychological, pharmacological and other common interventions for treatment of chronic musculoskeletal pain. It was based upon three systematic reviews and was developed by an APA guideline development panel composed of scientists, clinicians, and client/community representatives. All interested individuals and groups are invited to comment, including psychologists, health care professionals, researchers, clients/patients and their families, APA governance members, and the general public.
The American Psychological Association (APA) is currently accepting public comments on its Draft APA Clinical Practice Guideline for the Treatment of Chronic Musculoskeletal Pain in Adults. The guideline focuses on recommendations for psychological, pharmacological and other common interventions for treatment of chronic musculoskeletal pain. It was based upon three systematic reviews and was developed by an APA guideline development panel composed of scientists, clinicians, and client/community representatives. All interested individuals and groups are invited to comment, including psychologists, health care professionals, researchers, clients/patients and their families, APA governance members, and the general public.
Interested in Providing Your Thoughts? AACIPM has received an invitation to comment on these guidelines. While we are putting together our response, we would be happy to hear from you regarding your thoughts on the draft guideline. Please share your feedback with amy@painmanagementalliance.org by November 17.
All comments must be submitted no later than 11:59 pm, Eastern Time, on Monday, December 4, 2023.
VA Launches Study on Group-Based Psychological Treatments via Teleconference for Older Veterans with Chronic Pain
 Current guidelines for treating chronic pain from the U.S. Department of Veterans Affairs (VA) emphasize psychological treatments as first-line therapy, yet most currently available options have only been shown to provide modest benefits. To increase effectiveness, the VA will be conducting a four year study to test a number of treatment options, including Emotional Awareness and Expression Therapy (EAET), group and video telehealth delivered treatments, and identification of mechanisms of response so that the most effective treatments are selected for each patient. The trial focuses on older Veterans, a currently understudied subset of patients living with chronic pain. Following the trial, the VA plans to share resources on treatments, findings, and lessons learned with both VA clinicians and the broader scientific community.
Current guidelines for treating chronic pain from the U.S. Department of Veterans Affairs (VA) emphasize psychological treatments as first-line therapy, yet most currently available options have only been shown to provide modest benefits. To increase effectiveness, the VA will be conducting a four year study to test a number of treatment options, including Emotional Awareness and Expression Therapy (EAET), group and video telehealth delivered treatments, and identification of mechanisms of response so that the most effective treatments are selected for each patient. The trial focuses on older Veterans, a currently understudied subset of patients living with chronic pain. Following the trial, the VA plans to share resources on treatments, findings, and lessons learned with both VA clinicians and the broader scientific community.
Administration on Aging Fully Funds Eight Chronic Disease Self-Management Education Programs
 Aimed at providing older adults and adults with disabilities with education and tools to help them better manage chronic conditions such as diabetes, heart disease, arthritis, chronic pain, and depression, Chronic Disease Self-Management Education (CDSME) programs have been supported by the Administration on Aging (AoA) for the past twenty years. Grantees provide a number of activities and community services through use of these grants, including: partnering with local agencies on aging, local health departments, rural clinics, and hospitals; implementing self-management programs people living with chronic pain and opioid abuse/misuse; and, securing reimbursement via Medicare, Medicare Advantage, and Medicaid.
Aimed at providing older adults and adults with disabilities with education and tools to help them better manage chronic conditions such as diabetes, heart disease, arthritis, chronic pain, and depression, Chronic Disease Self-Management Education (CDSME) programs have been supported by the Administration on Aging (AoA) for the past twenty years. Grantees provide a number of activities and community services through use of these grants, including: partnering with local agencies on aging, local health departments, rural clinics, and hospitals; implementing self-management programs people living with chronic pain and opioid abuse/misuse; and, securing reimbursement via Medicare, Medicare Advantage, and Medicaid.
In 2023, the AoA awarded 8 fully-funded cooperative agreements totaling nearly $5 million. New grantees include programs located in Michigan, Georgia, Mississippi, New Mexico, New York, and Texas.
ICYMI
Telemedicine Temporary Rules to Expire November 11
In May, the U.S. Drug Enforcement Administration (DEA) and Substance Abuse and Mental Health Services Administration (SAMHSA) issued a temporary rule that extended telemedicine flexibilities adopted during the COVID-19 Public Health Emergency. Beginning November 11, 2023, these flexibilities will no longer apply to new patients seeking telemedicine. However, for any practitioner-patient telemedicine relationships that have been or will be established up to November 11, 2023, the full set of telemedicine flexibilities regarding prescription of controlled medications established during the COVID-19 PHE will be extended for one-year—through November 11, 2024.
Message from the Director
 Here we are entering the final two months of 2023! I hope this newsletter finds all of you well and with time for self-care during these busy times.
Here we are entering the final two months of 2023! I hope this newsletter finds all of you well and with time for self-care during these busy times.
I’m very enthusiastic about our next webinar on December 7 and hope that you will register and share this information with your networks. We also have a survey that is an important advocacy tool for connecting feedback from patients and providers with CMS and other policymakers. The survey results will be shared during the webinar so that we can identify action steps.
Implementation is the key to positive change and we want to help promote the uptake of comprehensive integrative pain management for all people.
Onward and Upward!
Amy
Relevant Reading
![]()
Emotional responses to favorite and relaxing music predict music-induced hypoalgesia, Frontiers in Pain Research, October 25
Nature exposure therapy for pediatric patients with chronic pain, Contemporary Pediatrics, October 20
What Is Whole Person Health? A Beginner’s Guide to the Interconnectedness of Body, Mind, and Your Environment, Everyday Health, October 19
Mindfulness Should Not Be Taught in School? Really?, Psychology Today, October 18
PODCAST: Millions of people have unexplained chronic pain. Can scientists help?, Economist, October 18
Comprehensive Programs Are Needed to Address Therapeutic Needs in Sickle Cell Disease, OncLive, October 12
How to make workplaces more inclusive for people with invisible disabilities, Fast Company, October 1
A Randomized, Controlled Neuroimaging Trial of Cognitive-Behavioral Therapy for Fibromyalgia Pain, American College of Rheumatology, September 20
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.
