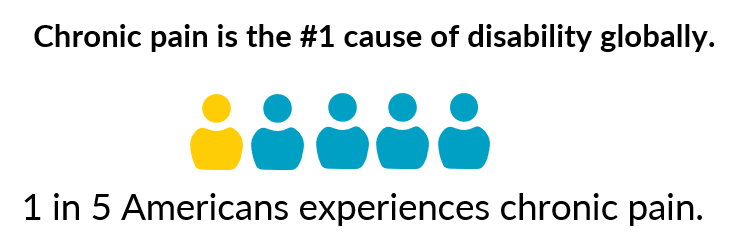
New CDC Report Reveals Chronic Pain Affects More Than 1 in 5
After a similar report in 2016, the CDC has released new study data about the prevalence of chronic pain in its Morbidity and Mortality Weekly Report on April 23, 2023. Chronic pain continues to affect more than one in five U.S. adults. This report included more details such as pain prevalence was higher in adults who were American Indian or Alaska Native, who identified as bisexual, or who were divorced or separated, the researchers said.
During 2021, an estimated 51.6 million adults (20.9%) had chronic pain lasting 3 months or longer, and 17.1 million (6.9%) had high-impact chronic pain — pain severe enough to restrict daily activities — reported S. Michaela Rikard, PhD, of the CDC’s National Center for Injury Prevention and Control, and co-authors.
What are the Implications for Public Health?
“Clinicians, practices, health systems, and payers should vigilantly attend to health inequities and ensure access to appropriate, affordable, diversified, coordinated, and effective pain management care for all persons,” Rikard and colleagues wrote.
NH Governor Signs Integrative Pain Care Bill!
House Bill 66
 You may remember Rep. David Nagel, MD, who we featured last November, as a new Representative in the state of New Hampshire. He is working hard in many ways, and one of these ways is a bill he co-wrote, HB 66, which the Governor signed on April 27, 2023!
You may remember Rep. David Nagel, MD, who we featured last November, as a new Representative in the state of New Hampshire. He is working hard in many ways, and one of these ways is a bill he co-wrote, HB 66, which the Governor signed on April 27, 2023!
Rep. Nagel shared with AACIPM Director his excitement and said, “My big goal is to include a variety of stakeholders and, most importantly, to have the patient at the center of this process – something often overlooked. With a committee process, we will develop an integrative model to empower patients in a patient-centered manner to manage their pain.”

Last Call for Scholarships for Providers Caring for Underserved
Integrative Pain Management Conf. May 5th, 2023
We are excited to see the list of providers who have received scholarships and represent many different disciplines and practice settings! To grow and strengthen the CIPM workforce, AACIPM is thrilled to collaborate with IM4US and UVM to offer scholarships to providers caring for the underserved, who are unable to attend without this support.
Scholarship Application Deadline: There is a hard deadline of 8am EDT on May 4, 2023 for virtual attendance. If we hear from you by then, you will receive a code to register right away.
Register Now
Specifically designed to meet the needs of an interdisciplinary health care community, the Second Integrative Pain Management Conference will be held on May 5, 2023, presented by The Osher Center for Integrative Health.
- General Public $275
- Students $125

Spain Passes Law Allowing Paid Menstrual Leave for Painful Periods
 Hailed as a historic step for feminist rights, Spain has become the first European country to pass a law that allows employees with painful periods to take paid menstrual leave from work. If a patient provides a doctor’s note, the law creates a right to a three-day menstrual leave of absence—with the possibility of extending it to five days—for those with disabling periods which can cause cramps, nausea, dizziness, and vomiting. The public social security system will fund the bill.
Hailed as a historic step for feminist rights, Spain has become the first European country to pass a law that allows employees with painful periods to take paid menstrual leave from work. If a patient provides a doctor’s note, the law creates a right to a three-day menstrual leave of absence—with the possibility of extending it to five days—for those with disabling periods which can cause cramps, nausea, dizziness, and vomiting. The public social security system will fund the bill.
It is hoped that this new law will help to fight the shame, stigma, and fear associated with painful periods for the millions of employees who menstruate every day. While menstrual leave is not common in the United States, it has begun to gain popularity in parts of Afro-Eurasia. In addition to Spain, a number of other countries have adopted some form of menstrual leave policy, including Japan, Indonesia, South Korea, Taiwan, Vietnam, and Zambia.
National Updates
X-Waiver No Longer Needed but DEA Implements New Education Requirements
 The x-waiver requirement, which restricted who may treat patients with buprenorphine for opioid use disorder, will be officially rescinded effective June 21, 2023. The Consolidated Appropriations Act of 2023 removes the requirement, and there will no longer be any limits or caps on the number of patients that a prescriber may treat for opioid use disorder with buprenorphine (existing state laws and regulations will remain in effect). Prescribers will only need a DEA registration number to treat patients for OUD.
The x-waiver requirement, which restricted who may treat patients with buprenorphine for opioid use disorder, will be officially rescinded effective June 21, 2023. The Consolidated Appropriations Act of 2023 removes the requirement, and there will no longer be any limits or caps on the number of patients that a prescriber may treat for opioid use disorder with buprenorphine (existing state laws and regulations will remain in effect). Prescribers will only need a DEA registration number to treat patients for OUD.
While the x-waiver will no longer be required to treat OUD, new or renewing DEA registrants will be required to have met at least one of the following criteria effective June 27, 2023:
- Eight hours of training on opioid or other substance use disorders;
- Board certification in addiction medicine or addiction psychiatry from the American Board of Medical Specialties, American Board of Addiction Medicine, or the American Osteopathic Association; or
- Graduation within five years and status in good standing from medical, advanced practice nursing, or physician assistant school in the United States that included successful completion of an opioid or other substance use disorder curriculum of at least eight hours.
FDA Updates Prescribing Information for IR and ER/LA Pain Medicines
 The FDA is requiring several updates to the prescribing information for both immediate-release (IR) and extended release/long acting (ER/LA) opioid pain medicines. Updates for patients, parents, and caregivers include information on taking opioid medications exactly as prescribed, safe and secure storage, seeking help in the event of respiratory problems, and talking to health care professionals about the benefits of naloxone and how to obtain it. Health care professionals are advised to: prescribe the lowest effective dose of an IR opioid for the shortest duration of time to reduce the risks associated with these products; reserve ER/LA opioid pain medicines only for severe and persistent pain that requires an extended treatment period with a daily opioid pain medicine and for which alternative treatment options are inadequate; discuss naloxone with patients; and more.
The FDA is requiring several updates to the prescribing information for both immediate-release (IR) and extended release/long acting (ER/LA) opioid pain medicines. Updates for patients, parents, and caregivers include information on taking opioid medications exactly as prescribed, safe and secure storage, seeking help in the event of respiratory problems, and talking to health care professionals about the benefits of naloxone and how to obtain it. Health care professionals are advised to: prescribe the lowest effective dose of an IR opioid for the shortest duration of time to reduce the risks associated with these products; reserve ER/LA opioid pain medicines only for severe and persistent pain that requires an extended treatment period with a daily opioid pain medicine and for which alternative treatment options are inadequate; discuss naloxone with patients; and more.
NAM Hosts 4-Part Series on Improving Telehealth and Virtual Care for Pain Management and Substance Use Disorders
 In an effort to better understand both the challenges and opportunities for telehealth and virtual care within the pain management and SUD care ecosystems, the Opioid Action Collaborative’s Working Groups on Pain Management Guidelines and Evidence Standards (PM) and Prevention, Treatment, and Recovery Services (PTR) convened a four-party meeting series as a forum to explore both the barriers and opportunities for expanding telehealth and virtual care services in pain management and OUD/SUD care. The series has worked to identify key barriers and opportunities for expanding telehealth and virtual care services for pain and OUD/SUD, including actionable and evidence-informed guidance that can support future decision-making by policymakers, regulators, payers, health systems, clinicians, and patients.
In an effort to better understand both the challenges and opportunities for telehealth and virtual care within the pain management and SUD care ecosystems, the Opioid Action Collaborative’s Working Groups on Pain Management Guidelines and Evidence Standards (PM) and Prevention, Treatment, and Recovery Services (PTR) convened a four-party meeting series as a forum to explore both the barriers and opportunities for expanding telehealth and virtual care services in pain management and OUD/SUD care. The series has worked to identify key barriers and opportunities for expanding telehealth and virtual care services for pain and OUD/SUD, including actionable and evidence-informed guidance that can support future decision-making by policymakers, regulators, payers, health systems, clinicians, and patients.
Message from the Director
 The new survey data released from CDC for 2019-2021 shows that the prevalence of chronic pain continues to affect more than one in 5 people or 21% of our adult population. This doesn’t even include people under 18 and veterans who are often underserved and struggling to get whole person, multimodal pain management.
The new survey data released from CDC for 2019-2021 shows that the prevalence of chronic pain continues to affect more than one in 5 people or 21% of our adult population. This doesn’t even include people under 18 and veterans who are often underserved and struggling to get whole person, multimodal pain management.
As we address the lack of equitable access to BioPsychoSocialSpiritual pain care, many discussions keep turning to digital technologies and opportunities. We will share more about this in the next issue of our newsletter as we continue to advocate for equitable care for all.
If you haven’t already, I hope you will view and share the registration information for the UVM conference (virtual option) taking place on May 5 in Burlington, VT. This is one of numerous important successes out there that brings a comprehensive integrative approach to pain care — this one with a bundled payment through BC/BS of Vermont.
Onward and Upward!
Amy
Relevant Reading
![]()
Addressing chronic disease requires holistic, personalized approach to care, Medical Economics, April 27
Obesity & Pain Management: A Primary Viewpoints Podcast, Patient Care, April 27
Dispelling the Myths Behind Palliative Care, Michigan Medicine, April 27
Music therapy found to significantly reduce pain, stress and anxiety in community hospitals, Medical Xpress, April 26
Alcohol Fuels Pain: Study Reveals Link Between Drinking and Chronic Pain, Neuroscience News, April 22
‘Intelligent and kind’ Truro woman who had ‘factitious’ symptoms took own life because of the pain, Cornwall Live, April 19
As Pandemic Emergency Ends, People with Long Covid Feel Abandoned, Pain News Network, April 18
Acupuncture Can Improve Sleep for Cancer Survivors With Chronic Pain, Cure, April 18
Turning Down the Volume of Pain: How to Retrain Your Brain When You Get Sensitized, Neuroscience News, April 16
Five VA apps that help Veterans and their families manage stress, VA News, April 15
Chronic Pain Affects 21% of Americans, CDC Reports— Nearly 7% have pain severe enough to restrict daily activities, MedPage Today, April 13
First Pediatric Pain Management Standard Published in Canada, Medscape, April 13
How virtual reality can help relieve chronic pain, Medical Xpress, April 11
5 Ways to Avoid Scrutiny in Pain Management Codes, Practical Pain Management, April 6
VA expands virtual reality for Veteran rehabilitation, VA News, April 3
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.

