Improving the Transition from Military Service Member to Veteran through Quality Comprehensive Well-Being Experiences
Reflecting on how the VA and DoD are working together to connect the dots for the men and women who serve our nation.
By Amy Goldstein, Director, AACIPM
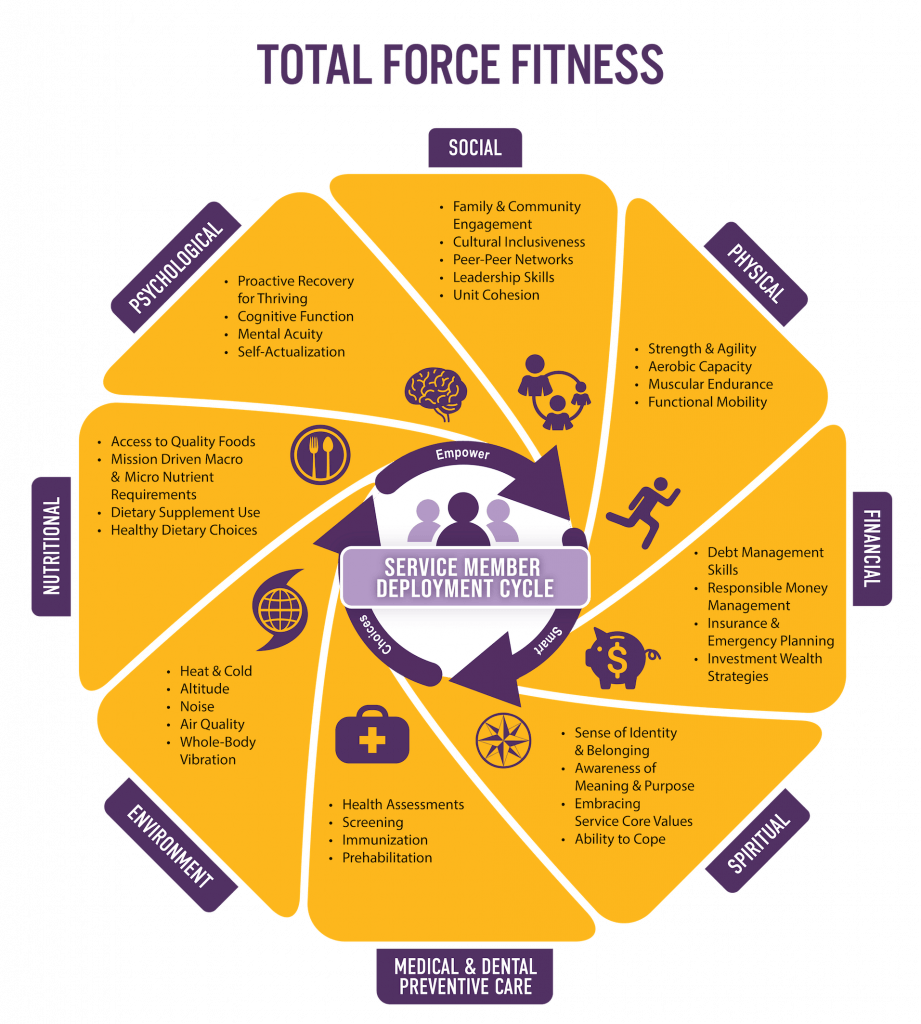
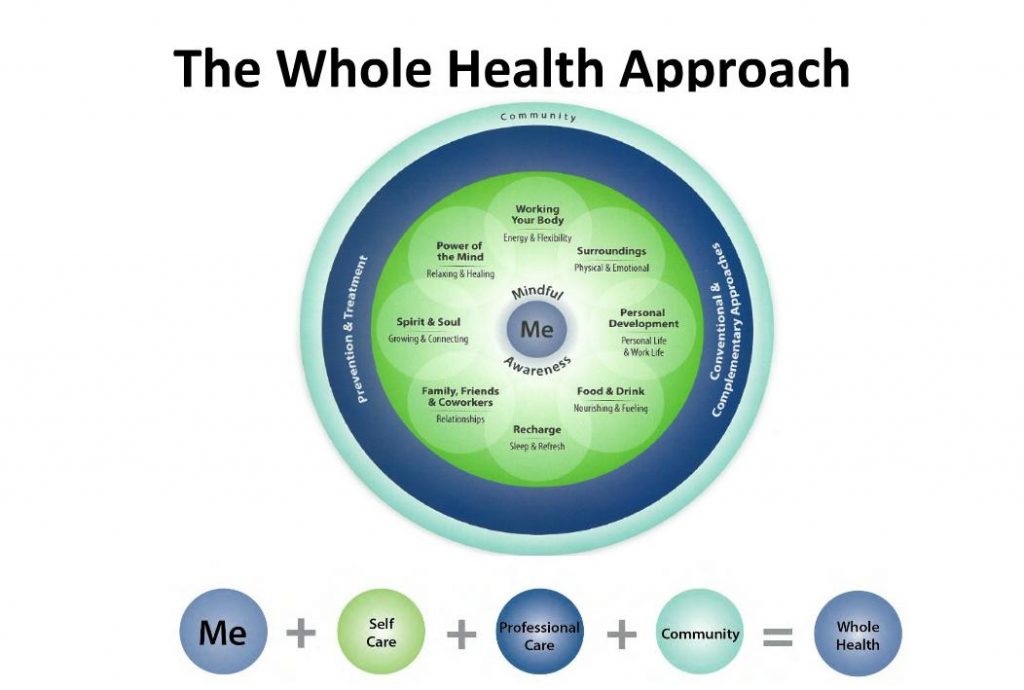
 I recently had the honor to participate in the Total Force Fitness (TFF) – Whole Health (WH) Summit, a two-day summit held jointly by the Department of Defense (DoD) and Department of Veterans Affairs (VA) from March 22-23 at the Uniformed Services University. The meeting was co-organized/co-facilitated by one of AACIPM’s Advisory Committee members, Eric Schoomaker, MD, PhD, FACP, Lieutenant General, US Army (Ret), and by Melissa “Missy” Givens, MD, Colonel US Army (Ret), the director of the Consortium for Health and Military Performance which was instrumental in developing the DoD’s TFF concept a decade ago. The goal of this important summit was to discuss how DoD’s Total Force Fitness and VA’s Whole Health programs can align opportunities for improving the comprehensive well-being and resilience of Service Members and Veterans. Specifically, the summit focused on the pivotal transition from DoD to VA comprehensive well-being programs, including health promotion and healthcare.
I recently had the honor to participate in the Total Force Fitness (TFF) – Whole Health (WH) Summit, a two-day summit held jointly by the Department of Defense (DoD) and Department of Veterans Affairs (VA) from March 22-23 at the Uniformed Services University. The meeting was co-organized/co-facilitated by one of AACIPM’s Advisory Committee members, Eric Schoomaker, MD, PhD, FACP, Lieutenant General, US Army (Ret), and by Melissa “Missy” Givens, MD, Colonel US Army (Ret), the director of the Consortium for Health and Military Performance which was instrumental in developing the DoD’s TFF concept a decade ago. The goal of this important summit was to discuss how DoD’s Total Force Fitness and VA’s Whole Health programs can align opportunities for improving the comprehensive well-being and resilience of Service Members and Veterans. Specifically, the summit focused on the pivotal transition from DoD to VA comprehensive well-being programs, including health promotion and healthcare.
The question to be answered was this: How can DoD’s TFF and VA’s WH be optimally linked for the benefit of the Transitioning Service Member (AKA, the new Veteran)? Over the course of two days, we heard from dozens of presenters representing all aspects of the DoD and VA, each describing how their program, services, and/or research related to Total Force Fitness and Whole Health. Through these individual presentations, we could see the similarities in construct and intent between the two programs–a holistic approach to well-being (e.g., physical, social, financial, spiritual, environmental, etc.).
Read more to see the linkages with whole person, multimodal pain management.
AMA’s Story: Putting the “Multi” in Multimodal Care for Patients with Pain
An example of integrative pain care from American Medical Association
 AACIPM thanks one of our many collaborators, International Association of Yoga Therapists (IAYT), who introduced us to Inner Atlas, a unique method of facilitating whole person, multimodal pain care led by Whitney James, MD, MHS, Kori Moore-Gibson, C-IAYT and Malisa Szalkiewicz, M.ED, C-IAYT.
AACIPM thanks one of our many collaborators, International Association of Yoga Therapists (IAYT), who introduced us to Inner Atlas, a unique method of facilitating whole person, multimodal pain care led by Whitney James, MD, MHS, Kori Moore-Gibson, C-IAYT and Malisa Szalkiewicz, M.ED, C-IAYT.
As a connector of dots to promote whole person-centered pain care, AACIPM has collaborated with the AMA to share this example across many stakeholders.
While many people talk about the mind-body connection as part of optimal care for patients with pain, Arizona physician Whitney James, MD, has gone a step further, developing her own program to make that the guiding principle in how she treats patients.
In her own words, Dr. James discusses her practice philosophy and how she built a strong team to help her put her vision into practice:
“It’s been my experience that patients with chronic pain are best treated with a multimodal treatment plan. This may include a combination of physical therapy, talk therapy, medications and even surgery. No two patients are alike, so each patient’s treatment plan must be individualized to her or his unique physiology and experience. What doesn’t tend to work well with chronic pain patients is a single angle approach. Practitioners really need to be able to create multifaceted treatment plans in order to be effective in improving patient outcomes and quality of life.”
Read the story on AMA’s microsite, titled Putting the ‘Multi’ in Multimodal Care for Patients with Pain.
Reach out to AACIPM if you want to share unique models of caring for people with pain.

WHITNEY JAMES, MD, MHS

KORI MOORE-GIBSON, C-IAYT

MALISA SZALKIEWICZ, M.ED, C-IAYT


National Updates
 Congress Considers Payment for Non-opioids in the NOPAIN Act
Congress Considers Payment for Non-opioids in the NOPAIN Act
The Non-Opioids Prevent Addiction in the Nation Act (NOPAIN Act) has been introduced in the Senate. If passed, this bill would temporarily establish Medicare reimbursement for a period of five years for certain drugs, biologics, and devices used for pain management that are able to replace or reduce opioid consumption, as shown through clinical trials or data. The bill would also require CMS to submit a report to Congress identifying the limitations, gaps, barriers to access, or deficits in Medicare coverage or reimbursement for restorative therapies, behavioral approaches, and complementary and integrative health services that are identified in the Pain Management Best Practices Inter-Agency Task Force Report.
The NOPAIN Act was introduced on March 4th by Senators Rob Portman, Jeanne Shaheen, Shelley Moore Capito, and Joe Manchin, and has been referred to the Committee on Finance.
Deadline for Responding to CDC and FDA Draft Guidance is April 11 CDC continues to accept public comments on CDC Clinical Practice Guideline for Prescribing Opioids—United States, 2022. AACIPM is currently working with a writing group made up of varied stakeholder organizations and experts to develop a collective response. If you are a leader of an organization or policy group interested in learning more about this effort, contact Amy Goldstein, Director, AACIPM.
CDC continues to accept public comments on CDC Clinical Practice Guideline for Prescribing Opioids—United States, 2022. AACIPM is currently working with a writing group made up of varied stakeholder organizations and experts to develop a collective response. If you are a leader of an organization or policy group interested in learning more about this effort, contact Amy Goldstein, Director, AACIPM.
 FDA continues to accept feedback from the public on their draft Development of Non-Opioid Analgesics for Acute Pain. The guidance provides recommendations about three specific topics: development of non-opioid analgesic products for acute pain, labeling claims, and expedited programs as they pertain to this purpose.
FDA continues to accept feedback from the public on their draft Development of Non-Opioid Analgesics for Acute Pain. The guidance provides recommendations about three specific topics: development of non-opioid analgesic products for acute pain, labeling claims, and expedited programs as they pertain to this purpose.
Public comments are due for both dockets no later than April 11, 2022.
Appropriations Update: FY 2022 Budget Finalized, Increases Health Funding After numerous congressional delays, President Joe Biden signed the Consolidated Appropriations Act, 2022 (H.R. 2471) into law on March 15, 2022. The law completes all funding bills for federal agencies for FY 2022, including finalization of the NIH Budget.
After numerous congressional delays, President Joe Biden signed the Consolidated Appropriations Act, 2022 (H.R. 2471) into law on March 15, 2022. The law completes all funding bills for federal agencies for FY 2022, including finalization of the NIH Budget.
The bill impacts healthcare in a number of ways, including, but not limited to:
- $45 billion for NIH in FY 2022, an increase of $2.03 billion over FY 2021.
- $50 million for health disparities research at National Institute on Minority Health and Health Disparities.
- $16.2 million to the Office of the Chief Officer for Scientific Workforce Diversity, an increase of $10 million over FY 2021 levels, to continue to lead efforts to combat racism and improve diversity in the biomedical research workforce.
- $541 million for the All of Us precision medicine initiative.
- $350 million for the Agency for Healthcare Research and Quality (AHRQ), an increase of $12.4 million above the FY 2021 spending level.
- $799 million for the Health Resources and Services Agency (HRSA) Title VII Health Professions and Title VIII Nursing Workforce Development Programs, a 5% increase above FY 2021 levels.
- $8 million for the CDC Social Determinants of Health Pilot Program.
With the budget now finalized, federal agencies are poised to release a large number of funding opportunities that were pending, subject to the final appropriations bill. NIH has already cleared a number of important pain-related research concepts for funding, and it is strongly recommended that stakeholders explore these possible funding opportunities prior to seeing official notices posted for them.
NIH and NIDA Continue to Fund Various Pain-related Projects
Funding opportunities related to pain management, integrative care, and other related topics continue to abound.
 The NIH HEAL Initiative currently has open funding opportunities related to:
The NIH HEAL Initiative currently has open funding opportunities related to:
- Availability of Administrative Supplements to Support Strategies to Increase Participant Diversity, Inclusion and Engagement in Clinical Studies (Application Due 04/29)
- Research Supplements to Promote Diversity in Health-Related Research (Admin Supp – Clinical Trial Not Allowed) (Application Due 05/15)
- Discovery and Functional Evaluation of Human Pain-Associated Genes and Cells (LOI Due 6/07)
- Discovery of Biomarkers and Biomarker Signatures to Facilitate Clinical Trials for Pain Therapeutics (LOI Due 05/24)
- Discovery and Validation of Novel Targets for Safe and Effective Pain Treatment (LOI Due 5/02)
![]() NIDA is currently aiming to fund:
NIDA is currently aiming to fund:
- Public Health Research on Cannabis, including impact of polysubstance use on health outcomes, including interactions (substitution/complementation) of cannabis product use with alcohol, tobacco, and prescription and nonprescription opioids. (Begins accepting applications June 5, 2022)
New Resource
 NCCIH has released a new fact sheet, Qigong: What You Need to Know.
NCCIH has released a new fact sheet, Qigong: What You Need to Know.
Qigong, pronounced “chi gong,” is a practice from China that involves using exercises to optimize energy within the body, mind, and spirit, with the goal of improving and maintaining health and well-being.
Most forms of qigong combine breathing exercises, smooth movements, and mental focus. Some qigong techniques are dynamic (active), with an emphasis on body movements, while others are meditative (passive), focusing on breathing and mental exercises.
Qigong may be helpful for balance training and fall prevention. A small amount of research suggests that qigong may be helpful for symptoms of some chronic diseases, such as fibromyalgia and chronic obstructive pulmonary disease.
Read the new fact sheet to learn more about this ancient practice and its health effects.
Message from the Director
 Happy Spring! It’s such a beautiful time of year and I especially loved that my trip to Washington, DC last week coincided with seeing the cherry blossoms. You can read my reflections about the VA and DoD’s Total Force Fitness-Whole Health Summit I attended in this newsletter.
Happy Spring! It’s such a beautiful time of year and I especially loved that my trip to Washington, DC last week coincided with seeing the cherry blossoms. You can read my reflections about the VA and DoD’s Total Force Fitness-Whole Health Summit I attended in this newsletter.
As things continue to bloom, so are we, at AACIPM, focused on strengthening these connections. This month, you’ll see the story from AMA – the third piece they have released about integrative pain care (see more here). Also, AACIPM is

busy working on a group response to the CDC’s request for comment on their new guidelines for prescribing opioids, which is due by April 11.
More resources are in development and will be shared in the forthcoming issues. As always, please reach out with any feedback or ideas.
Onward and Upward!
Amy
Relevant Reading
![]() Chronic low back pain associated with regional brain atrophy, News Medical, March 29
Chronic low back pain associated with regional brain atrophy, News Medical, March 29
Music therapy helps patients with sickle cell disease cope with pain, Healio, March 29
Chronic Pain Makes You Think Differently, Discover Magazine, March 28
The pandemic gave people with chronic illnesses a sense of belonging. Now they’re back to feeling like outsiders., Insider, March 20
What is myofascial release therapy?, Live Science, March 16
Mindfulness Therapy Can Reduce Chronic Pain and Opioid Misuse, Psychology Today, March 15
People Keep Telling Me I’m ‘Too Young To Be Sick.’ Here’s What They Don’t Understand., Huff Post, March 13
The Scientific Benefits of Meditation: Head to Heart, Body to Mind, Nebraska Central, March 11
Could Virtual Reality Replace Your Next Pain Pill?, US News and World Report, March 10
Endometriosis: Why is there so little research?, Medical News Today, March 10
Updated CDC Prescription Opioid Guidelines Appear More Flexible And Patient-Centric, But Fall Short, Forbes, March 4
Impact of a Multimodal Analgesia Protocol in an Intensive Care Unit: A Pre-post Cohort Study, Cureus, March 3
Meghan O’Rourke on the Self-Dissolving Difficulty of Chronic Illness, Lit Hub, March 3
Does nerve damage contribute to ‘long-COVID’ symptoms?, Science Daily, March 2
Pelvic Pain: The Pain Problem with No Home, Practical Pain Management, March 1
Research: The Link Between Recessions and Physical Pain, Harvard Business Review, March 1
Behavioral Medicine: Lifestyle Interventions to Reduce Inflammatory Pain, Practical Pain Management, March 1
Peripheral Neuropathy Evaluations of Patients With Prolonged Long COVID, Neurology, Neuroimmunology & Neuroinflammation, March 1
Study on Types of Pain in MM Reveals Communication Inadequacies Between Physicians, Patients, AJMC, February 28
Invisible: Living with Behcet’s disease, Medical News Today, February 28
Podcast: Long COVID, Chronic Illness & Searching For Answers, NPR, February 28
Podcast: How long COVID sheds light on other mysterious (and lonely) chronic illnesses, NPR, February 28
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.
The Connector – March 2022
0 Comments
Submit a Comment
Sign up to receive our updates

0 Comments