Pain Realities
Our country is in a time of change and innovation in pain management, as many stakeholders are responding to an increased emphasis on providing safe, high-quality, evidence-informed, individualized pain care.
As efforts to combat opioid misuse and overdose continue, we must not overlook the fact that some of the roots of the opioid epidemic lie in inadequately managed pain. Today, 50 million Americans suffer from untreated pain, half of whom are living with pain that significantly impairs their ability to go about their daily lives. This includes over 22 million people who are still employed and trying to manage their symptoms. Chronic pain negatively affects a person’s quality of life, and has also been shown to impact social environments and mental health. Patients need access to safe and effective treatments to manage their pain.
Context
Chronic pain is the #1 cause of disability globally.
1 in 6 Americans lives in pain every day.
Nearly 20 million Americans have pain that prevents life activities and work.

Annual expenses and lost productivity
Consensus
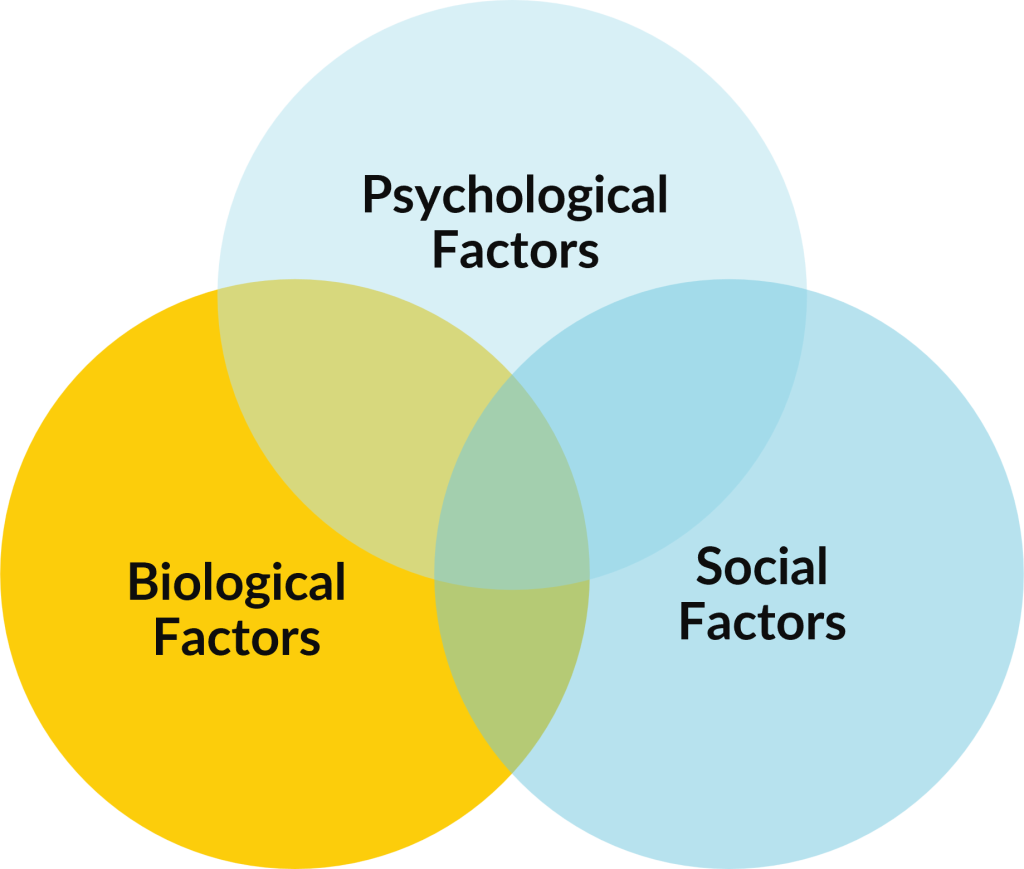
- The BioPsychoSocial Model is foundational to person-centered care and pain management.
- Most clinical guidelines recommend non-pharmacological, low-risk treatments as first-line treatment for pain.
- Individualized, evidence-based, integrative, multi-modal is the gold standard of care.
CHallenge
Evidence based, guideline-concordant, multimodal care is not accessible for many people, especially those who are underserved.

Misperceptions & Stigma
People with pain, and the clinicians who treat them, often face both hidden and obvious stigma from family, friends, coworkers, and the health care system.

Lack of Public Awareness
Pain is complex and quality pain care requires a solid understanding of all options within the pain management toolbox. This requires a culture change in which the patient’s various providers work together on a collaborative treatment plan and/or make adequate use of referrals when the patient may benefit from supplemental treatment from another professional.

Business Case Data Disagreement
Payors and providers often disagree about which models of care are both scalable and sustainable. To fully understand the effectiveness of patient-centered, multimodal pain interventions, it is imperative to analyze pragmatic trials, comparative effectiveness studies, healthcare utilization data, and cost analyses, in addition to randomized controlled trials.

Workforce Supply & Demand
In addition to an overall provider shortage that is only worsening, there is an extreme shortage of an array of licensed and certified healthcare providers that effectively represent BIPOC communities. Further, there is inadequate training and interprofessional knowledge that keeps healthcare providers from understanding what it means to provide a multimodal, multidisciplinary approach to pain care.

Misaligned Financial Incentives
Achieving value-based care requires creative adjustment to current payment structures. Fee-for-service can make access to a multimodal approach quite difficult, while bundled payment models may be difficult to sustain. Provider/Payor and other non-traditional partnerships are needed to increase access to a variety of evidence-based therapies in all geographic locations.

Integration & Cultural Incompatibilities
Integration of conventional clinical care and complementary and integrative health is complicated. Differences in provider approaches result from cultural barriers when trying to bring these approaches together, and developing a collaborative pain care plan can be difficult when providers do not work within the same health system and/or use the same electronic health record system.
Conclusion
AACIPM connects the dots to advance equitable, whole person, multi-modal pain care.
- People with Pain
- Payers / Purchasers
- Healthcare Providers
- Policymakers
- Academia / Researchers
- Government Agencies
- Advocates
- Caregivers / Family
