Fostering Connections During NIH HEAL Investigator Meeting

Dr. Shari Ling, CMS with Amy Goldstein, AACIPM
On February 21st and 22nd, the NIH HEAL Initiative brought together HEAL funded researchers, federal officials, people with lived experience, and other stakeholders to share research findings, explore trends and shared interests, and identify opportunities to advance the goals of the initiative. Thank you to Isabel Roth, DrPH, MS, for inviting AACIPM’s Director, Amy Goldstein, to attend as a Community Advisory Board member for the OPTIMUM study looking at mindfulness for chronic low back pain in primary care. The meeting included panels, scientific symposia, discussion groups, networking, and poster sessions for in-person and virtual attendees.
After the meeting, Amy Goldstein said:
“This was my first NIH HEAL meeting. Besides being inspiring and productive, it also felt very important to foster deeper dot-connecting with various leaders who participate in aspects of person-centered, evidence-based pain management but do not have the space to share and collaborate. Keeping individuals with pain at the center of efforts is not easy. Patient abandonment, suicide rates and overdoses are at an all time high (in parallel with the decrease in opioid prescribing), part of the devastating unintended consequences when we try to address a complex public health challenge. AACIPM stakeholders seek tangible opportunities to address real-world implementation and dissemination strategies, and continue connecting more dots!”

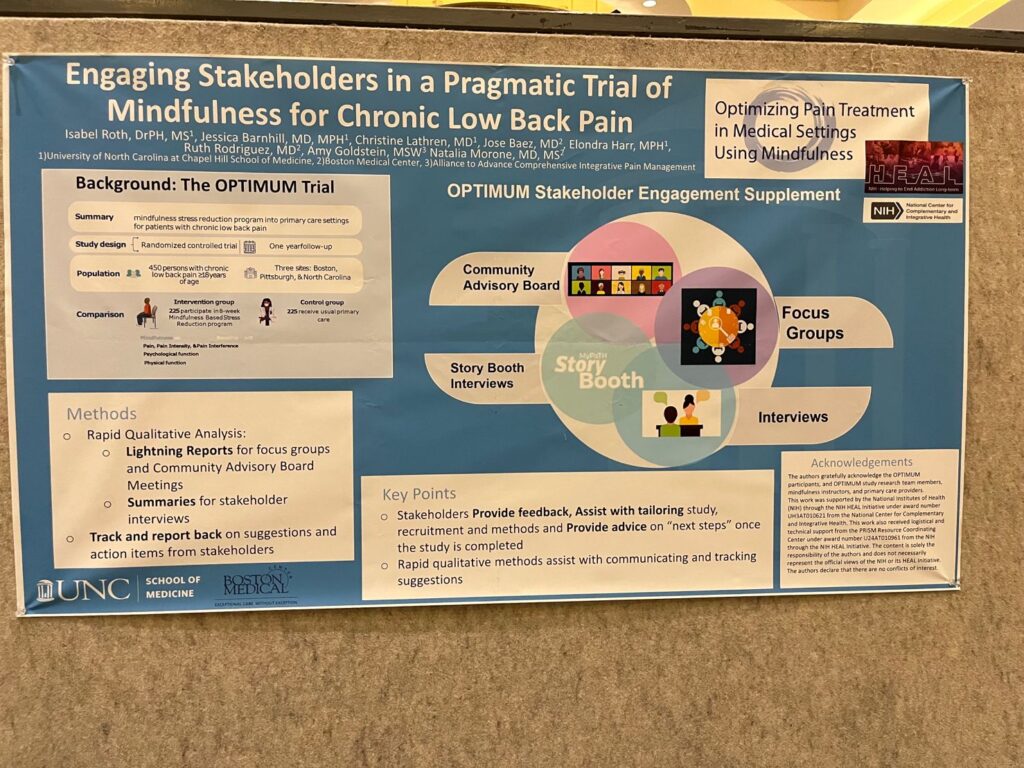
Amy Goldstein with poster presentation, pictured with Natalia Morone, MD (Boston Medical Center) and Isabel Roth, DrPH, University of NC at Chapel Hill School of Medicine.
AACIPM’s Webinar on Rethinking CIPM Transformed Perspectives and Motivated Change
 On January 25th, AACIPM presented its webinar: Realities, Research & Rethinking Person-Centered, Integrative Pain Management. Most clinical guidelines recommend that non-pharmacological therapies should be first line treatments, yet, this approach to care remains elusive for many people based on numerous pain realities. Directly confronting this disconnect, AACIPM brought together perspectives from people with pain, research, clinical practice and payers to discuss innovation and progress in their field and how to keep people with pain at the center of this care.
On January 25th, AACIPM presented its webinar: Realities, Research & Rethinking Person-Centered, Integrative Pain Management. Most clinical guidelines recommend that non-pharmacological therapies should be first line treatments, yet, this approach to care remains elusive for many people based on numerous pain realities. Directly confronting this disconnect, AACIPM brought together perspectives from people with pain, research, clinical practice and payers to discuss innovation and progress in their field and how to keep people with pain at the center of this care.
The exciting results from AACIPM’s post-webinar survey have revealed that the opinions and knowledge base of those who attended was significantly impacted by the information shared:
- 50% changed their opinion on the value of person-centered comprehensive integrative pain management.
- 77% changed their opinion on the current body of evidence recommending complementary and integrative treatments for pain management, with attendees claiming to be more certain of CIPM’s value, more informed by current information and resources, and encouraged to see a growing body of evidence in support of CIPM.
- 68% are motivated to act or do something differently based upon their participation in the webinar, including: incorporating the provided resources into their practice; working to update and coordinate their own care plans as patients; teaching clinical students to better listen to patient stories; holding more compassion for patients living with pain; and, collaborating more with other provider types.
Replays of the webinar are now available on our website.
National Updates
 NCCIH Releases Summary of the Stakeholder Meeting for Research on Whole Person Health
NCCIH Releases Summary of the Stakeholder Meeting for Research on Whole Person Health
As a follow-up to their October meeting, NCCIH has released a meeting summary of their Stakeholder Meeting for Research on Whole Person Health. The meeting, which was attended by AACIPM Director Amy Goldstein, posed three questions for discussion:
- Why does complementary and integrative health need a unifying concept?
- What is whole person health?
- What are the goals of this meeting?
The meeting was attended by delegates representing acupuncture, yoga therapy, chiropractic, osteopathic medicine, physical therapy, somatic movement therapy, massage therapy, physicians’ assistants, nursing, naturopathic medicine, homeopathy, Ayurvedic medicine, energy psychology, music therapy, integrative health organizations, patient advocacy and research organizations, and government organizations.
Amy participated in the two-day stakeholder meeting and also offered testimony on behalf of AACIPM in regard to closing the gap to advance access to guideline-concordant integrative care.
 VA Makes Chronic Pain Management More Accessible via TelePain
VA Makes Chronic Pain Management More Accessible via TelePain
The Veterans Administration is working to make pain management services more accessible to veterans through new TelePain programs being built at multiple VA health care systems throughout the country. The first TelePain program, piloted by VA Northwest Network’s Clinical Resource Hubs (CRH) TelePain team, has provided interdisciplinary pain care to over 900 Veterans in the last nine months. Using a veteran-centered approach, the programs virtually connect veterans living with pain to interdisciplinary teams that work to address all aspects of pain management, including mental health care, nutrition, occupational therapy, and medication.
In addition, VA’s Health Services Research and Development Service will present Comorbid Chronic Pain and PTSD: The Case for Yoga as a Simultaneous Treatment, a cyber seminar, on March 7, 2023. This presentation will review the state of the science on yoga for chronic pain, PTSD, and their co-occurrence and discuss clinical implications and future directions for research.
National Cancer Institute: Study Finds Disparities in Access to Opioids for Cancer Pain at End of Life
![]() According to a study that looked at opioid prescriptions filled from 2007 to 2019, Black and Hispanic patients with cancer received fewer opioids and at lower doses than White patients. The study did not identify the cause of these differences, but the differences were seen even when researchers considered factors such as people’s income levels and where they lived. The study covered the years since the US opioid epidemic was recognized, which resulted in tighter regulation of opioid prescribing and changes in public and health care provider attitudes about opioids. Study authors conclude that an unintended consequence of the new laws and regulations is that it has become much harder for people with cancer to get pain medications, despite guidelines that recommend opioids for the treatment of moderate to severe pain from cancer or cancer treatment.
According to a study that looked at opioid prescriptions filled from 2007 to 2019, Black and Hispanic patients with cancer received fewer opioids and at lower doses than White patients. The study did not identify the cause of these differences, but the differences were seen even when researchers considered factors such as people’s income levels and where they lived. The study covered the years since the US opioid epidemic was recognized, which resulted in tighter regulation of opioid prescribing and changes in public and health care provider attitudes about opioids. Study authors conclude that an unintended consequence of the new laws and regulations is that it has become much harder for people with cancer to get pain medications, despite guidelines that recommend opioids for the treatment of moderate to severe pain from cancer or cancer treatment.
New CMS Pain Codes – Moving to Dissemination and Implementation
 In case you missed it last month, CMS has released new pain codes, effective Jan. 1, 2023. There are different perspectives among participants in this multi-stakeholder collaborative, and it’s very important to the AACIPM team that we continue to capture what is happening where the rubber meets the road for people living with pain.
In case you missed it last month, CMS has released new pain codes, effective Jan. 1, 2023. There are different perspectives among participants in this multi-stakeholder collaborative, and it’s very important to the AACIPM team that we continue to capture what is happening where the rubber meets the road for people living with pain.
To continue to spread awareness of these codes, and to aid in their uptake, AACIPM has compiled a number of helpful resources below. Keep in mind this is early in the process, so there’s a lot to think about in terms of dissemination and implementation in the coming months.
- CMS Pain Management Codes for 2023
- Calendar Year (CY) 2023 Medicare Physician Fee Schedule Final Rule | CMS
- CMS Creates New Pain Management Codes Heeding Advice of AACIPM – Alliance to Advance Comprehensive Integrative Pain Management
- Reimbursement for Chronic Pain Management in the 2023 Medicare Physician Fee Schedule: New Opportunities for Patients and Providers — Nixon Gwilt Law.
- The Centers for Medicare and Medicaid Services (CMS) Makes a Major Move to Improve Pain Care – U.S. Pain Foundation
- CMS Pain Management Codes for 2023 – Practical Pain Management
You will see there are a number of issues being raised in the links above, and we will be curating more information around this as we continue engagement with CMS and other stakeholders.
To this end, please share any feedback you have in regard to the following questions and/or any other issues or aspects you are seeing in regard to the codes:
- Is your clinic adjusting to implement use of these codes? If yes, are there questions or concerns being raised that aren’t currently addressed in the communications?
- Is there incentive to use these codes as they are described?
- As currently coded (not a “Designated Care Management Service”), clinical staff time may not be billed incident to a physician’s services where outsourced clinical staff is not in the same physical location as the physician. Are you able to capture the need for this “incident to” billing, so that, if needed, we can share this information with CMS more readily?
- Do you have any experience yet with using the codes in patient care? If yes, how is that working?
- CMS added the CPM codes to the Medicare Telehealth list despite requiring the initial visit to take place in person at a clinic. With unknowns about future legislation around telehealth services, we are interested in capturing the effect this might have on using the codes.
We look forward to hearing from all of you regarding your use of these codes and/or the barriers you experience regarding their use. Please contact Amy Goldstein with any feedback.
Partner Education Highlights
Pediatric Pain Warrior Family Summer Camp
 The U.S. Pain Foundation is hosting the second annual Pediatric Pain Warrior Family Summer Camp. The five-day summer camp will be held at Morgan’s Wonderland Camp in San Antonio, Texas, from June 25 to June 29, 2023. Morgan’s Wonderland Camp is an Ultra-Accessible™ camp with a particular emphasis on giving people with physical and developmental disabilities an opportunity to enjoy summer-camp-type activities alongside guests without special needs.
The U.S. Pain Foundation is hosting the second annual Pediatric Pain Warrior Family Summer Camp. The five-day summer camp will be held at Morgan’s Wonderland Camp in San Antonio, Texas, from June 25 to June 29, 2023. Morgan’s Wonderland Camp is an Ultra-Accessible™ camp with a particular emphasis on giving people with physical and developmental disabilities an opportunity to enjoy summer-camp-type activities alongside guests without special needs.
So, why are we sharing this information? This is an opportunity to support their efforts and get involved. Examples of ways to collaborate include:
- Sharing news about the camp to your communities — The application for camp is open until March 8.
- Swag Bags — Every family receives a welcome bag of goodies, snacks, products, and resources when they arrive. All items need to arrive by May 15.
- Scholarship/Financial Support — Sponsor a family. On average, the five-day camp costs an estimated $1,500 per family of four.
AAPM Podcast Explores Racial Disparities in Pain Medicine
 The current medical system is fraught with racial prejudices and misunderstandings that often lead to unequal treatment across the healthcare system. In honor of Black History Month, the American Academy of Pain Medicin’s Pain Matters Podcast presented Under the Microscope – Examining Racial Disparities in Pain Medicine with Aderonke Pederson, M.D.
The current medical system is fraught with racial prejudices and misunderstandings that often lead to unequal treatment across the healthcare system. In honor of Black History Month, the American Academy of Pain Medicin’s Pain Matters Podcast presented Under the Microscope – Examining Racial Disparities in Pain Medicine with Aderonke Pederson, M.D.
Interested in helping to bridge the treatment gap?
Tune in to discover:
- The history of racial exploitation in the U.S. healthcare system
- How racial biases impact the treatment of pain in black patients
- The implications of racial disparities on the black experience
How physicians can address disparities in pain treatment

Integrative Pain Management Conference
Join an interdisciplinary group of colleagues for a day of:
- Learning best practices, research, and innovations in integrative approaches for chronic pain management
- Exploring ways to provide integrative chronic pain treatment to medically underserved populations
- Understanding policy initiatives focused on increasing access to integrative, comprehensive pain treatments
- Discovering techniques that can be integrated into day-to-day clinical practice
- Networking with and learning from an interdisciplinary group of colleagues
Early Bird Prices until April 1, 2023
Message from the Director
 It has been really wonderful to reconnect with so many fantastic colleagues and leaders during recent travel. I enjoyed the NIH Heal Investigator’s meeting in Washington, DC (see the update in this newsletter).
It has been really wonderful to reconnect with so many fantastic colleagues and leaders during recent travel. I enjoyed the NIH Heal Investigator’s meeting in Washington, DC (see the update in this newsletter).
Today I’ve arrived in Chicago for the Academic Consortium for Integrative Medicine and Health – here’s a picture of me with Dr. Vanila Singh (left) before her plenary with Dr. Shari Ling on The Intersection of Integrative Medicine, Health Policy and Advancing Care in Chronic Painful Conditions. I know this conference will also be inspiring and spark numerous connections.
Also, please share any feedback you might have regarding the new pain codes from CMS (see more information on this in National Updates above.)
Onward and Upward!
Amy
Relevant Reading
![]()
Mindfulness and Chronic Musculoskeletal Pain: An Umbrella Review, Dovepress, February 28
Animal Study Offers Clues to the Link Between Sleep and Chronic Pain, Practical Pain Management, February 28
Researchers say pain is undertreated in nursing home residents, McKnights, February 27
Radically Accepting Chronic Pain, Psychology Today, February 26
Making chronic pain management care more accessible, VA News, February 23
Pain Self-Efficacy Is an Important Quality-of-Life Mediator in Migraine, Clinical Pain Advisor, February 23
Opinion Today: A new way to understand — and treat — pain, NY Times, February 23
Making chronic pain management care more accessible, VA News, February 23
Piriformis Syndrome in Pre-monsoon, Monsoon, and Winter: An Observational Pilot Study, Cureus, February 22
Elevated dementia risk, cognitive decline, and hippocampal atrophy in multisite chronic pain, PNAS, February 21
Dementia risk rises if you live with chronic pain, study says, CNN, February 20
Vulvodynia: What it is, symptoms, treatment and more, Medical Xpress, February 20
“I can see light, I got hope”: Veteran gets second chance at life through pain management program, ABC 36, February 17
70 Best Pain Management Blogs and Websites, FeedSpot, February 16
Is Pain Treated Effectively With Antidepressants?— Review calls for nuanced approach to treating pain conditions, MedPage Today, February 1
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.
