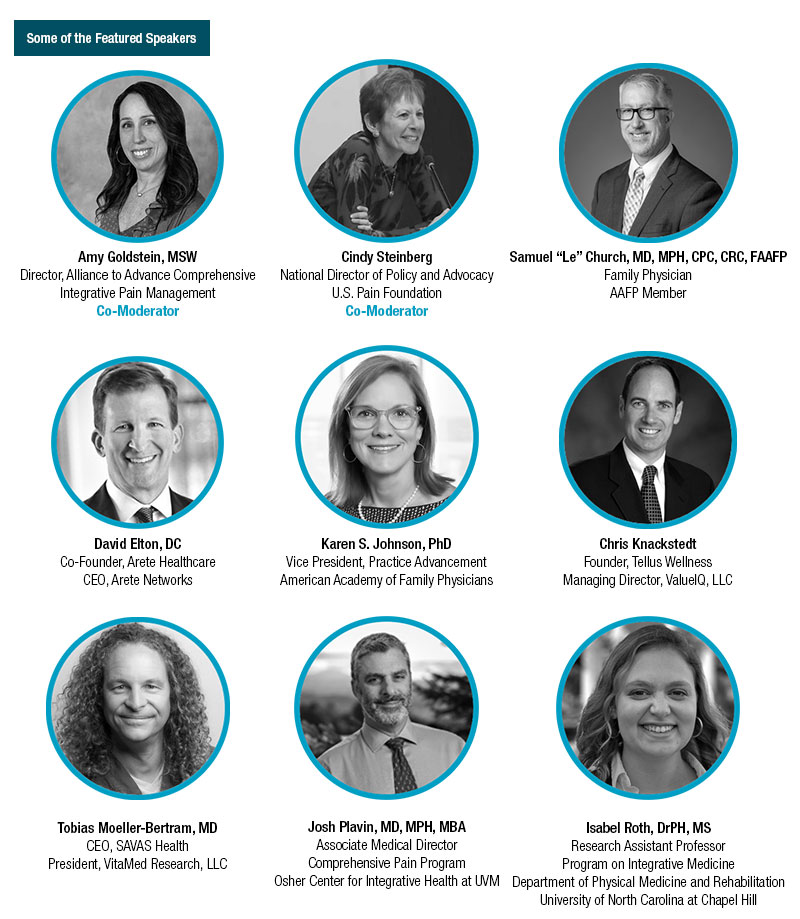
Join a MultiStakeholder Discussion About:

On behalf of the Alliance to Advance Comprehensive Integrative Pain Management and the US Pain Foundation, we invite you to join this lively and constructive discussion about the intersection of payer policies and person-centered, value-based care delivery for high-impact pain.
This discussion will include perspectives from people with pain, payors, providers, purchasers, academia, policymakers, industry, and more.
In light of CMS’ laudable goal for Medicare and Medicaid beneficiaries to be in value-based care relationships by 2030, we will discuss the real-world impact of this goal. Our esteemed panelists (see their bios) each bring a unique perspective and practical expertise to the conversation with an understanding of the nuances of how payer policies impact clinical—and scalable—implementation of pain care.
Participants in this free webinar will learn about:
- CMS efforts to advance value-based care, including the new CMS pain codes – what these are, what they mean, and how the first year since their release is going.
- What person-centered, evidence-based, multimodal, pain care is – and what scalable and value-based really means.
- Public and private sector innovation advancing access to transdisciplinary pain care for people who are underserved.
- Value-based care innovation that offers a network of chiropractors, acupuncturists, nutritionists, massage therapists, health coaches, and naturopaths.
- An example of family practice in rural Georgia and how the CMS codes impact value-based care delivery.
Whether or not you can attend the webinar, your feedback is crucial to webinar development, so please take a few minutes to complete this survey and/or share it with your networks.
National Updates
NHIS Data Shows Opioid Use for Chronic Pain is Down with No Corresponding Increase in Nonpharmacologic Therapies
According to Prevalence of Pharmacologic and Nonpharmacologic Pain Management Therapies Among Adults with Chronic Pain—United States, 2020, recently published in the Annals of Internal Medicine, prescription opioid use for chronic pain decreased from 15.2% in 2019 to 13.5% in 2020. However, despite current CDC guidelines that recommend maximizing the use of alternative therapies in place of opioid therapy when possible, there was no corresponding increase in nonpharmacologic therapies.
The paper analyzed results from the annual National Health Interview Survey (NHIS) and had a number of other key takeaways:
- 60% of adult respondents used a combination of pharmacologic and nonpharmacologic treatments for pain and almost 27% used medications alone.
- Those least likely to turn to nonpharmacologic treatment for pain include older adults, those with low incomes, uninsured individuals, and those living in the South.
Of the respondents taking medications, 76% self-reported using over-the-counter pain relievers for pain, followed by prescription nonopioids (31%) and prescription opioids (13.5%).
 AACIPM to Respond to American Psychological Association’s Solicitation of Public Comment on Draft Guidelines for Chronic Musculoskeletal Pain in Adults
AACIPM to Respond to American Psychological Association’s Solicitation of Public Comment on Draft Guidelines for Chronic Musculoskeletal Pain in Adults
The American Psychological Association (APA) is currently accepting public comments on its Draft APA Clinical Practice Guideline for the Treatment of Chronic Musculoskeletal Pain in Adults. The guideline focuses on recommendations for psychological, pharmacological and other common interventions for treatment of chronic musculoskeletal pain. It was based upon three systematic reviews and was developed by an APA guideline development panel composed of scientists, clinicians, and client/community representatives. All interested individuals and groups are invited to comment, including psychologists, health care professionals, researchers, clients/patients and their families, APA governance members, and the general public.
AACIPM has received an invitation to comment on these guidelines. After convening a number of stakeholders representing patients, health care providers, payers, and more, AACIPM is now putting together a group response to the proposed guidelines. For more information, contact Amy Goldstein.
All comments must be submitted no later than 11:59 pm, Eastern Time, on Monday, December 4, 2023.
 CMS Releases Finalized Physician Fee Schedule for 2024
CMS Releases Finalized Physician Fee Schedule for 2024
The Centers for Medicare & Medicaid Services (CMS) have released the final rule addressing changes the physician fee schedule (PFS) for 2024.
While some commenters during the public comment period had requested that CMS add the General Behavioral Health Integration (GBHI) code and the Chronic Pain Management (CPM) codes into the weighted average for the calculation of HCPCS code G0511, CMS has once again stated that they will only revisit the valuation issue after actual utilization becomes available.
Further, CMS is adding five new episode-based measures to their cost performance category, one of which is Low Back Pain, beginning with the CY 2024 performance period/2026 MIPS payment year. The intent of the Low Back Pain measure is to assess the treatment and management of Low Back Pain and the triggering logic was designed to capture the range of clinicians that have a role in treating and managing this condition.
 Updated National Survey on Drug Use and Health Released by SAMHSA
Updated National Survey on Drug Use and Health Released by SAMHSA
The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), has released the results of the 2022 National Survey on Drug Use and Health. Showing how Americans are living with mental health, substance use, and treatment-related behaviors, the data will inform knowledge, policy, and action throughout the government and the healthcare industry.
Key findings from 2022 include:
- 17.3% of people aged 12 or older had a substance use disorder (SUD) in the past year.
- 23.1% of adults aged 18 or older had any mental illness (AMI) in the past year.
- 19.5% of adolescents aged 12 to 17 had a past year major depressive episode (MDE).
- 1 in 20 adults aged 18 or older, and over 1 in 8 adolescents aged 12 to 17, had serious thoughts of suicide in the past year.
SAMHSA Seeks to Fund Programs Addressing Behavioral Health Challenges in Local Communities
The Substance Abuse and Mental Health Services Administration (SAMHSA) has announced notices of funding opportunities for grant programs that address behavioral health challenges in local communities by preventing substance use initiation, reducing the progression of substance use, and addressing other related concerns. Totaling $74.4 million, the grant opportunities include:
- Expansion and Sustainability of the Comprehensive Community Mental Health Services for Children with Serious Emotional Disturbances (CMHI) to provide resources to improve the mental health outcomes for children and youth, birth through age 21, at risk for or who have serious emotional disturbances, and their families.
- Tribal Behavioral Health to prevent and reduce suicidal behavior and substance use/misuse, prevent overdose, reduce the impact of trauma, and promote mental health among American Indian/Alaska Native youth, up to and including age 24, by building a healthy network of systems, services, and partnerships that impact youth.
- Strategic Prevention Framework – Partnerships for Success for States to reduce the onset and progression of substance misuse and its related problems by supporting the development and delivery of state and community substance misuse prevention and mental health promotion services.
- Strategic Prevention Framework – Partnerships for Success for Communities, Local Governments, Universities, Colleges, and Tribes/Tribal Organizations to reduce the onset and progression of substance misuse and its related problems by supporting the development and delivery of community-based substance misuse prevention and mental health promotion services.
 DEA and HHS Extend Temporary Telemedicine Rules Through 2024
DEA and HHS Extend Temporary Telemedicine Rules Through 2024
In May 2023, the U.S. Drug Enforcement Administration (DEA) and Substance Abuse and Mental Health Services Administration (SAMHSA) issued a temporary rule that extended telemedicine flexibilities adopted during the COVID-19 Public Health Emergency. Previously set to expire on November 11, 2023, the temporary rule has now been extended again to last through December 31, 2024 in order to avoid lapses in care for patients.
![]() NIDA Offers Resources on Screening for Substance Use in the Pain Management Setting
NIDA Offers Resources on Screening for Substance Use in the Pain Management Setting
On behalf of the National Institute on Drug Abuse (NIDA), Dr. Steven Stanos, DO has offered a number of tips and resources for screening pain patients for risky substance use and expert guidance on what to do if patients with pain screen positive for unhealthy substance use. Guidance includes screening for substance use in a health care provider’s workflow, utilizing the state prescription drug monitoring program (PDMP), selecting screening and assessment tools and risk stratification tools, tools for managing patient comorbidities, inclusion of the patient’s family members in the screening process (with the patient’s permission), and creating a list of behavioral health providers to use when referrals are in the best interest of the patient.
Partner Educational Offerings

Clinical Care Options 9th Annual Psychopharmacology Update
December 8-9 | In-Person and Online | 7:00am-4:00pm ET | JW Marriott Orlando
Featured Talk: “Applying Best Practices in Pain Management”
Access a diverse range of topics, including major depressive disorder, bipolar depression, tardive dyskinesia, narcolepsy, and schizophrenia.
Register Now
Academic Consortium’s 2024 Congress on Integrative Medicine and Health
April 9-13 | Cleveland, OH
Learn More
American Academy of Pain Medicine’s 40th Annual Conference
March 7-10 | Scottsdale, AZ
Learn More
Message from the Director
 I hope this month’s issue finds you well. Please take a few minutes to read through the updates and let us know if you have relevant information to share that is missing. We are looking forward to making more updates to our newsletter in the coming year and always want to hear from you.
I hope this month’s issue finds you well. Please take a few minutes to read through the updates and let us know if you have relevant information to share that is missing. We are looking forward to making more updates to our newsletter in the coming year and always want to hear from you.
I hope to see you at our upcoming webinar on December 7 – I know this will be of interest to many of you as we explore the intersection of payor policy and practice. We must talk about how to scale equitable, value-based pain care and learn from those already engaged in this work.
Onward and Upward!
Amy
Relevant Reading
![]()
What Is Ableism? The Sneaky Assumption That Hurts Disabled People, Yahoo! Life, November 26
Analgesic Use in Primary Care, MedCentral, November 16, 2023
Acupuncture vs Massage for Pain in Patients Living With Advanced CancerThe IMPACT Randomized Clinical Trial, JAMA Network Open, November 14
A Bibliometric Analysis of Acupuncture Therapy in the Treatment of Musculoskeletal Pain from 2003 to 2022, Dovepress, November 13
Guarding and flow in the movements of people with chronic pain: A qualitative study of physiotherapists’ observations, European Journal of Pain, November 7
The endocannabinoid N-arachidonoyl dopamine is critical for hyperalgesia induced by chronic sleep disruption, Nature Communications, October 25
A Quick Guide to Collaborative Care: How to Improve Outcomes, Reduce Costs, and Get Paid, MedCentral, October 4, 2023
Reattribution to Mind-Brain Processes and Recovery From Chronic Back PainA Secondary Analysis of a Randomized Clinical Trial, JAMA Network Open, September 28
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.
