CMS Creates New Pain Management Codes Heeding Advice of AACIPM
![]() The Centers for Medicare & Medicaid Services (CMS) has issued its finalized 2023 Physician Fee Schedule, creating, for the first time, billing codes at the federal level that are specific to the delivery of chronic pain management (CPM) services. These codes (HCPCS G3002 and G3003) pertain to chronic pain lasting longer than three months, may be billed by a physician or other qualified health practitioner, and cover services including:
The Centers for Medicare & Medicaid Services (CMS) has issued its finalized 2023 Physician Fee Schedule, creating, for the first time, billing codes at the federal level that are specific to the delivery of chronic pain management (CPM) services. These codes (HCPCS G3002 and G3003) pertain to chronic pain lasting longer than three months, may be billed by a physician or other qualified health practitioner, and cover services including:
- administration of a validated pain rating scale or tool;
- the development, implementation, revision, and/or maintenance of a person-centered care plan that includes strengths, goals, clinical needs, and desired outcomes;
- overall treatment management;
- facilitation and coordination of any necessary behavioral health treatment;
- medication management;
- facilitation and coordination of any necessary behavioral health treatment;
- pain and health literacy counseling;
- any necessary chronic pain-related crisis care; and/or,
- ongoing communication and care coordination between relevant practitioners furnishing care (e.g. physical therapy and occupational therapy, complementary and integrative approaches, and community-based care), as appropriate.
SPOTLIGHT: Dr. Dave Nagel Talks Pain, Advocacy, and Spurring Change as a Newly Elected Representative
 Recently, AACIPM Director Amy Goldstein sat down with David Nagel, MD, long-time patient advocate, who was just elected on November 8 to represent Belknap 6 in the New Hampshire House of Representatives!
Recently, AACIPM Director Amy Goldstein sat down with David Nagel, MD, long-time patient advocate, who was just elected on November 8 to represent Belknap 6 in the New Hampshire House of Representatives!
AACIPM: How did you get involved with NFL PA (National Football League Players Association) , and what is important for us to understand about the Pain Management Guide that has been released?
Dr. Nagel: […] I was excited about this opportunity for several reasons. First, my first experience in advocacy was with post-concussive syndrome. When the NFL PA took this issue on, I was amazed by how much easier my work became, as I was able to win cases in court merely by citing the NFL. I thought that this could work similarly for pain care. Second, I had a vision of creating a consumer-oriented, evidence-based, pain care guide that would empower athletes, active and retired, with the knowledge they needed to manage their own care, and then use this model to trickle down to the general public. In order to do this, I interviewed athletes at all levels of participation, from pee-wee to elite. I was shocked to find out how little they trusted the medical staffs involved in their pain-care. Sound familiar? It became quite apparent there was a need for such a guide.
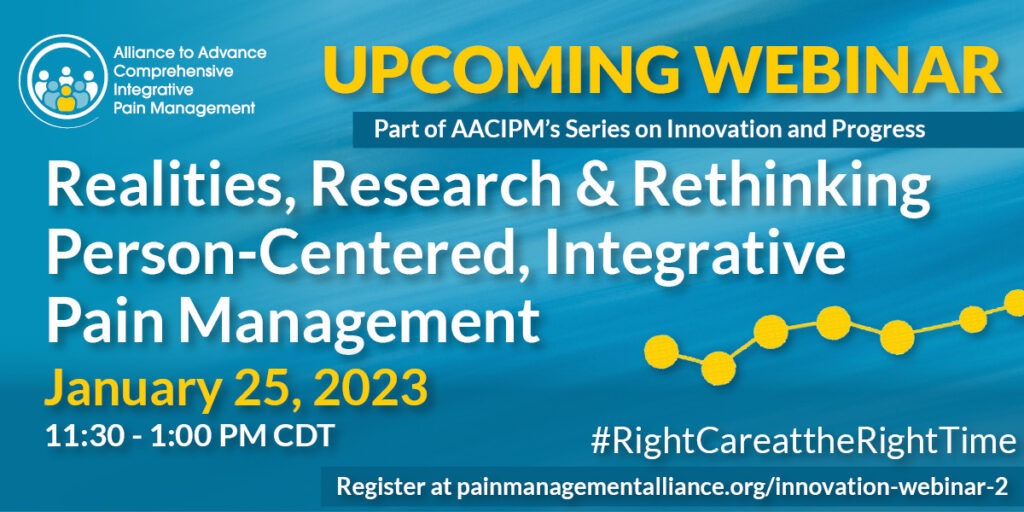
WEBINAR REGISTRATION OPEN
Realities, Research & Rethinking
Person-Centered, Integrative Pain Management
Wednesday, January 25, 2023, 11:30-1:00PM CDT
Most stakeholders agree that a person-centered, multimodal, integrative approach to pain care is best practice – and most clinical guidelines recommend that a non-pharmacological treatment should be tried first. Yet, this approach to care remains elusive for many people based on numerous pain realities. This webinar brings together perspectives from people with pain, research, clinical practice and payers to discuss innovation and progress in their field and how to keep people with pain at the center of this care.
Some presenters include:
- Dan Clauw, MD, Director, Chronic Pain & Fatigue Research Center, University of Michigan
- Doug Metz, DC, EVP & Chief Health Services Officer, American Specialty Health
- Beth Darnall, PhD, Director, Stanford Pain Relief Innovations Lab
- Bethany Ranes, PhD, Research Scientist
National Updates
CDC Expands Opioid Guidance to Include Acute Pain and Additional Providers
 The Centers for Disease Control and Prevention (CDC) has released its Clinical Practice Guideline for Prescribing Opioids for Pain (2022). Updated and revised, this new guidance is intended to replace the CDC’s 2016 opioid guideline. While the previous guideline was limited in scope to primary care providers treating chronic pain in adults, the new guidance has been broadened to provide evidence-based recommendations for prescribing opioid pain medication for acute, subacute, and chronic pain for outpatients aged ≥18 years, excluding pain management related to sickle cell disease, cancer-related pain treatment, palliative care, and end-of-life care. Further, and of vital importance, the CDC has made it explicitly clear that its guideline is intended to be voluntary and not to be used as an inflexible standard of care by health systems, insurers, or legislatures.
The Centers for Disease Control and Prevention (CDC) has released its Clinical Practice Guideline for Prescribing Opioids for Pain (2022). Updated and revised, this new guidance is intended to replace the CDC’s 2016 opioid guideline. While the previous guideline was limited in scope to primary care providers treating chronic pain in adults, the new guidance has been broadened to provide evidence-based recommendations for prescribing opioid pain medication for acute, subacute, and chronic pain for outpatients aged ≥18 years, excluding pain management related to sickle cell disease, cancer-related pain treatment, palliative care, and end-of-life care. Further, and of vital importance, the CDC has made it explicitly clear that its guideline is intended to be voluntary and not to be used as an inflexible standard of care by health systems, insurers, or legislatures.
NIDA Compiles Resources Related to Opioids and Pain Management
![]() The National Institute on Drug Abuse (NIDA) has released a resource compilation of general information and related resources on opioids, including an overview of how the U.S. Department of Health and Human Services (HHS) and the National Institutes of Health are taking steps to combat it. The resources include a number of national strategies and guidelines to tackle the crisis, including the newly updated CDC guideline (see above), the U.S. Surgeon General’s spotlight on opioids, the NIH HEAL Initiative’s news and research spotlights, the American Dental Association’s new policy to combat the opioid epidemic, as well as materials from CMS, FDA, and other branches of HHS.
The National Institute on Drug Abuse (NIDA) has released a resource compilation of general information and related resources on opioids, including an overview of how the U.S. Department of Health and Human Services (HHS) and the National Institutes of Health are taking steps to combat it. The resources include a number of national strategies and guidelines to tackle the crisis, including the newly updated CDC guideline (see above), the U.S. Surgeon General’s spotlight on opioids, the NIH HEAL Initiative’s news and research spotlights, the American Dental Association’s new policy to combat the opioid epidemic, as well as materials from CMS, FDA, and other branches of HHS.
NAM Releases Chronic Pain Journey Map
 The National Academy of Medicine (NAM) has released a new Chronic Pain Journey Map. The map is a visual illustration that intends to describe the diverse experiences of persons living with chronic, non-cancer, pain. The map identifies five key stages of the pain journey that have critical touchpoints with the health system, with each stage of the journey framed by lived experience perspectives. The map explains what works well, common challenges, and identifies actions that specific health care stakeholders (i.e. clinicians, health systems/payers, and chronic pain community organizations) can take to improve the pain management process.
The National Academy of Medicine (NAM) has released a new Chronic Pain Journey Map. The map is a visual illustration that intends to describe the diverse experiences of persons living with chronic, non-cancer, pain. The map identifies five key stages of the pain journey that have critical touchpoints with the health system, with each stage of the journey framed by lived experience perspectives. The map explains what works well, common challenges, and identifies actions that specific health care stakeholders (i.e. clinicians, health systems/payers, and chronic pain community organizations) can take to improve the pain management process.
HHS Promotes Equity through Enhanced Payment for Non-Opioids in Ambulatory Surgical Centers
![]() In accordance with the CMS opioid strategy, CMS will pay for five qualifying non-opioid pain management drugs when administered in ambulatory surgical centers in CY 2023. This ensures that Medicare beneficiaries have access to non-opioid pain management drugs and encourages providers to use non-opioids rather than opioids for pain management.
In accordance with the CMS opioid strategy, CMS will pay for five qualifying non-opioid pain management drugs when administered in ambulatory surgical centers in CY 2023. This ensures that Medicare beneficiaries have access to non-opioid pain management drugs and encourages providers to use non-opioids rather than opioids for pain management.
Message from the Director
 I hope each of you take a moment to read this issue and see what our collective advocacy efforts have helped to accomplish.
I hope each of you take a moment to read this issue and see what our collective advocacy efforts have helped to accomplish.
It’s also very exciting to spotlight David Nagel – a physician in New Hampshire that has taken his decades of advocacy work to a new level as a Representative in the state!
From the AACIPM team to you and your family, we wish you all the best in December.
Onward and Upward!
Amy
Relevant Reading
![]()
Mindfulness Pilot Study Hints at Benefits for hEDS, HSD Patients, Ehlers-Danlos News, November 28
Why Consider Physical Therapy for Migraine With Neck Pain?, Psychology Today, November 25
At least 76% Of People Who Have Long Covid Face Stigma Frequently, Forbes, November 25
Viewing chronic pain as its own illness is providing better treatments, NewScientist, November 16
Pain: The Great Motivator— Beth Darnall and Sean Mackey discuss behavioral health therapies for chronic pain management, MedPage Today, November 15
Study Confirms Memory, Concentration Issues After Lyme Disease, WebMD, November 15
Genicular nerve blocks provide short term pain relief for patients with knee osteoarthritis, News Medical Life Sciences, November 13
Researchers receive $3.2 million to study efficacy of mind-body practices in improving pain, surgical outcomes, EurekAlert! AAAS, November 10
Non-Opioid Pain Care Remains Out of Reach Due to Healthcare Disparities, Practical Pain Management, November 9
Exercise May Reduce Disability in Chronic Low Back Pain, Clinical Pain Advisor, November 4
Has Long COVID Always Existed? The pandemic might not have spawned a new chronic illness but rebranded an old one., NY Magazine, November 4
CDC Releases UPDATED Clinical Practice Guideline for Prescribing Opioids for Pain, CDC, November 3
Chronic pain: Evidence from the national child development study, PLOS One, November 2
Feedback
We welcome your input! What do you like? Do you have a contribution for an upcoming newsletter? Send us your comments, suggestions, or contributions.
