 After an illustrious 42-year career, including 240 publications and unparalleled advocacy in pain management, Charles (Chad) G. Helmick III, MD (CAPT, USPHS, RET) is officially retiring from CDC on December 31. It is with bittersweet hearts that we at AACIPM announce his retirement as Senior Medical Officer for the Division of Population Health at the Centers for Disease Control and Prevention (CDC), and the former scientific lead for CDC’s Arthritis Program, directing the program’s surveillance, epidemiology, and prevention research. Dr. Helmick has been a friend and ally to those in the pain management community for many decades, implementing arthritis and lupus programs at CDC, helping to craft the National Pain Strategy, and participating in the multi-stakeholder collaborative work of the Alliance to Advance Comprehensive Integrative Pain Management for many years. As a champion of encouraging interest in a public health approach to chronic pain, Dr. Helmick will be sorely missed, so we asked him a few questions about his time working with the CDC and what he envisions for the future of pain management policy.
After an illustrious 42-year career, including 240 publications and unparalleled advocacy in pain management, Charles (Chad) G. Helmick III, MD (CAPT, USPHS, RET) is officially retiring from CDC on December 31. It is with bittersweet hearts that we at AACIPM announce his retirement as Senior Medical Officer for the Division of Population Health at the Centers for Disease Control and Prevention (CDC), and the former scientific lead for CDC’s Arthritis Program, directing the program’s surveillance, epidemiology, and prevention research. Dr. Helmick has been a friend and ally to those in the pain management community for many decades, implementing arthritis and lupus programs at CDC, helping to craft the National Pain Strategy, and participating in the multi-stakeholder collaborative work of the Alliance to Advance Comprehensive Integrative Pain Management for many years. As a champion of encouraging interest in a public health approach to chronic pain, Dr. Helmick will be sorely missed, so we asked him a few questions about his time working with the CDC and what he envisions for the future of pain management policy.
We wish Dr. Helmick all the best in his retirement!
AACIPM: How would you describe your path and role with chronic pain over your time at CDC?
Dr. Helmick: Through training as a medical detective in CDC’s Epidemic Intelligence Service, I began my CDC career working on viral special pathogens (e.g., Lassa fever, rabies) and rickettsial diseases (e.g., Rocky Mountain spotted fever, Q fever), both domestic and internationally. After six years, I decided to focus on chronic diseases as less urgent, but more important, public health problems. I started the Arthritis and Lupus Programs at CDC, where the main outcomes of interest are reducing symptoms and improving function. When the Interagency Pain Research Coordinating Committee (IPRCC) was created in 2012, I jumped at the chance to be CDC representative, figuring that more attention to chronic pain would also help address arthritis and lupus symptoms. I’ve remained on the IPRCC since. At CDC and in the pain community, I’ve strived to emphasize the importance of public health, surveillance, and epidemiology to documenting the impact of chronic pain and gaining the resources commensurate with its impact. NIH and the excellent members of the IPRCC have helped educate me more about chronic pain and supported those efforts.
AACIPM: What did you find was most challenging in your work with pain?
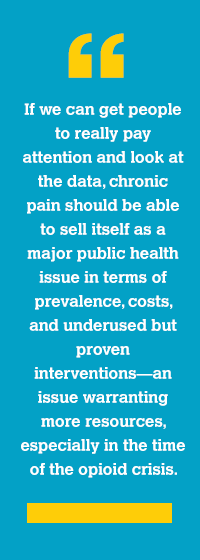
Dr. Helmick: CDC, the nation’s prevention agency, is the federal organization that responds to public health problems with prevention and control measures, including research. With such a large portfolio and relatively limited resources, it is challenging to add a new public health problem to the mix without having resources to support that effort. CDC’s opioid activities have some interest in chronic pain but mostly as it relates to opioids and not as a chronic disease problem it is own right. There has been slow but growing interest in principle in chronic pain as its own issue at CDC, but what is needed are resources, even minimal resources, that can get things started and be grown over time.
 AACIPM: What work are you most proud of?
AACIPM: What work are you most proud of?
Dr. Helmick: I’m extremely proud to have contributed to the IPRCC’s 2016 National Pain Strategy (NPS), which remains a useful guide on what to do next. Working with IPRCC colleagues, I was able to address several major objectives of the NPS:
- Use my experience with HHS’s Healthy People process (the nation’s health objectives) to quickly get pain objectives added to Healthy People 2020—a tangible achievement for the NPS. Pain objectives continue on Healthy People 2030.
- Create new chronic pain surveillance definitions and new prevalence estimates for both chronic pain in general and for high impact chronic pain (pain that interferes with work or life).
- Support growing interest by CDC’s National Center for Health Statistics in tracking pain in their current and future surveys, and developing the questions to use now and in the future.
AACIPM Editor’s Note: In the years before and after the release of the National Pain Strategy, we’ve seen the work of the National Academies of Medicine and the SUPPORT Act build upon the original Comprehensive Addiction & Recovery Act (CARA), as well as the release of the Pain Management Best Practices Inter-Agency Task Force Report. We believe these actions have promulgated the work of the NPS; yet many, especially those working at HHS, don’t fully understand the intricacies of each of these activities and how they interplay. See more about this here.
AACIPM: What advice would you give to stakeholders who are interested in chronic pain and public health?
Dr. Helmick: Persist in pursuing this perspective.The next steps for population research and interventions are laid out in the NPS by the working groups.
AACIPM: What will you be doing in retirement?
Dr. Helmick: After 49+ years in medicine and 42+ years in public health, I’m ready for more time with my hobbies (classic films, history, crosswords), family (my first two grandchildren this year!), and travel (when it becomes easier). I also stand ready to provide my high-level perspective on chronic pain and public health for those who are interested.
