AACIPM collaborated with stakeholders in support of CO House Bill 20-1085.
 “When patients are able to receive the types of care proposed in HB 20-1085, physical therapy, occupational therapy, chiropractic and acupuncture, they improve faster and the costs associated with their care go down,” said Amy Goldstein, Director, AACIPM during the public meeting. Furthermore, “in a review of Colorado insurance claims from 2018, Oliver Wyman found that 13% of patients treated for pain incurred over $2,500 per person in pain-related claims that year, and that these individuals had roughly eight times the healthcare costs of all remaining insured members.”
“When patients are able to receive the types of care proposed in HB 20-1085, physical therapy, occupational therapy, chiropractic and acupuncture, they improve faster and the costs associated with their care go down,” said Amy Goldstein, Director, AACIPM during the public meeting. Furthermore, “in a review of Colorado insurance claims from 2018, Oliver Wyman found that 13% of patients treated for pain incurred over $2,500 per person in pain-related claims that year, and that these individuals had roughly eight times the healthcare costs of all remaining insured members.”
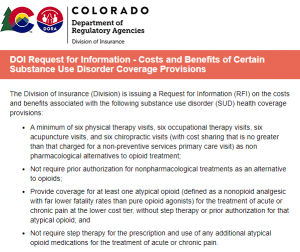
In 2018, Colorado passed legislation to establish a study committee related to opioid and other substance use disorders, and in 2019 that committee released a final report in which they formally recommended adoption of the bill that would ultimately become HB 20-1085. In 2020, that bill made it all the way to the Governor’s desk before being vetoed. The Governor has requested this RFI process to explore the impact of this bill on insurance premiums.
Trackbacks/Pingbacks