An interview with Diane Flynn, MD, primary care physician at Madigan’s Interdisciplinary Pain Management Center
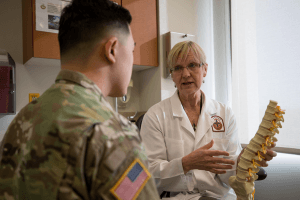
Dr. Diane Flynn, a physician in Madigan’s Interdisciplinary Pain Management Center at Joint Base Lewis-McChord, Wash., discusses available pain management treatments with her patient. Photo credit: Ryan Graham, Madigan Army Medical Center.
The Interdisciplinary Pain Management Centers (IPMC) at Madigan and at other Army Medical Centers were established in 2010 at the direction of the Army Medical Command and in response to the 2010 DOD/VA Pain Management Task Force (PMTF) Report. The PMTF was convened in 2009 with the mission of determining the best approaches for the management of pain, and its comprehensive report outlined 109 recommendations for pain management. Among the recommendations was the establishment of interdisciplinary pain centers to serve as tertiary care clinics and to provide support to military treatment facilities in each region. The Madigan IPMC provides tertiary pain management care to Joint Base Lewis-McChord (JBLM) and provides education and mentorship to military primary care teams throughout Washington, Alaska and California.
How is the IPMC different from traditional pain clinics?
The IPMC differs from traditional pain clinics in its truly interdisciplinary approach to addressing pain. In addition to interventional pain relieving procedures, the IPMC offers a broad array non-interventional pain therapies including physical and occupational therapy, psychology, medication management, chiropractic, acupuncture, yoga and massage. Real time collaboration leveraged synchronously among multiple disciplines is the key to interdisciplinary optimization of patient care and outcomes.
 What has been the greatest challenge in combining the mix of providers and disciplines that are on your team?
What has been the greatest challenge in combining the mix of providers and disciplines that are on your team?
The team based care in the IPMC is enjoyable for both clinicians and patients. In the early years of IPMC operation there was a learning curve as our clinical team learned more about one another’s disciplines. For example, acupuncturists use an approach to patient evaluation that is quite different from the approach used by clinicians trained through a Western medicine perspective. Over time, as we learned more about one another’s areas of expertise, we have adopted a common language that reinforces the value of a multimodal, interdisciplinary approach.
Describe the relationship that your IPMC has with primary care.
The Enhanced Community Health Outcomes (ECHO) program provides a vital interface with primary care. ECHO is a weekly tele-mentoring approach which involves a standard didactic curriculum and case-based teaching to specialty pain and primary care collaborators which has been shown to improve quality of care and reduce opioid risk. The IPMC also provides community outreach and education at the primary care level in order to inform primary care providers about available programs and services for patients struggling with pain. Three of the current IPMC providers have a background in primary care which facilitates the strong collaborative relationship we have with primary care teams in our region.
 Briefly describe how you see the importance of stepped care.
Briefly describe how you see the importance of stepped care.
The Stepped Care model of pain management is important to making high-quality pain care available to the maximum number of military patients. Stepped Care training emphasizes the important of patient self-management as the foundation of pain management. The Stepped Care model standardizes evaluation of pain among patients in primary care settings and encourages involvement of all members of the primary care team: Primary Care Clinician, nurses, embedded behavioral health providers and clinical pharmacists. The model provides guidance on when to refer patients to ancillary services such as physical therapy and when to refer to tertiary care.
Does your clinic impact patients in your facility (or region) that are never actually seen in your clinic?
Yes, IPMC clinicians provide guidance by email, phone call or through ECHO on the management of patients throughout the region. In addition, IPMC providers present didactic sessions to primary care clinics on Joint Base Lewis McChord.
Do providers and patients have difficulty with some of the modalities you provide as part of multi-modal pain management (acupuncture, movement therapy/Yoga…)?
When patients are evaluated in the IPMC, they are provided with several options for treatment, which may include self-management advice, a pain psychology program, medications, procedural interventions, or one of our three interdisciplinary programs. The SCOUT (Standard rehabilitative Care OUTpatient) program includes twice weekly physical and occupational therapy for six weeks; the REACH (REstorAtion through Complementary and integrative Health) program includes once-twice weekly chiropractic, acupuncture, yoga and massage for six weeks; and the intensive Functional Restoration Program includes 12 full days of PT, OT, pain psychology and education during a three week period. Once patients are offered these options they select which treatments in which they wish to engage. If patients do not like specific components of a treatment modality, the provider can adapt to another approach. For example, if patients are not comfortable with acupuncture needles, the acupuncturist can provide other approaches such as acupressure or cupping.

ECHO team in progress. Photo credit: Ryan Graham, Madigan Army Medical Center.
How have you traditionally used ECHO in your clinic and has it allowed you to do anything differently based on the realities of less face to face during this pandemic?
ECHO is a critical component of our outreach mission with specialty pain and primary care collaborators. Because ECHO uses a teleconferencing platform, we were able to continue ECHO sessions throughout the pandemic and positively influence patient outcomes while reducing potential patient exposure.
How has COVID19 impacted your clinic’s mission.
COVID-19 precautions had a major adverse impact on the ability of the IPMC to provide in-person pain care. The Madigan IPMC was closed to routine patient care for several months. This required creative solutions in order to meet the ongoing needs of our patients despite the unprecedented challenges of the COVID-19 global pandemic. During this timeframe virtual health was optimized and multiple efficiencies were realized that will allow enduring use of virtual health under appropriate circumstances well into the future. In July, we resumed patient care at half-capacity and we anticipate increasing to 75% capacity soon.

Wonderful interview! The emphasis on patient self-management as the foundation of pain management is right on!