 Finding comprehensive integrative pain management (CIPM) is as elusive as the prince finding his real princess who could feel the pea under the twenty mattresses! We are so grateful for the opportunity to share our lived experiences with the many stakeholders who joined us at the AACIPM Virtual Symposium. (click video below to view the recording).
Finding comprehensive integrative pain management (CIPM) is as elusive as the prince finding his real princess who could feel the pea under the twenty mattresses! We are so grateful for the opportunity to share our lived experiences with the many stakeholders who joined us at the AACIPM Virtual Symposium. (click video below to view the recording).
While we recounted our experiences from WTF to WOW, our stories continue. The quest persists. In this conversation, we’ll share with you what has worked for us, where we are now, and what we see as our tasks going forward.
First, let’s talk about what works. This list, while not exhaustive, is illustrative of the many different modalities we both found useful in our search for pain management: Kalind for the “suicide headaches” and Angel for the nerve and post-cancer treatment pain.
-
- Massage therapy
- Exercise
- Tai chi
- CBD products
- Vitamins/supplements
- Meditation
- Medication
- Nutrition counseling
- Education
- Family support
- Patient navigation
- Physical therapy
- Talk therapy
- Providers who practice active listening
What do you notice about this list?

Angel & Kalind Perry
Let me give you a hint: many of these therapies, in fact, most of them, are not covered by insurance. And of those covered by insurance, the co-pays and deductibles are often cost-prohibitive. We talk frequently in PAINS-KC about the financial burden of comprehensive integrative pain management being the number one barrier keeping many from accessing this vital treatment.
Since insurance is often tied to employment, let’s spend a moment talking about that. When Kalind had her first accident, it was covered by Workers’ Compensation (WC), but she was considered fit for duty—despite ongoing issues—two weeks after the injury. Her second accident also occurred on the job, but we’re not at liberty to talk about these since an open case still exists; it is sufficient to say, however, that having insurance tied to your employment can be both a benefit and a burden. We are grateful for all the medical care Kalind received through work-based insurance coverage, but that covered only a minimum of the expenses as she sought additional services on her own. Most of the CIPM was paid for out of our own reserves. We are fortunate that we are frugal by nature and had the resources; many families do not.
Eventually, Kalind found herself without a job, without insurance, without income, and living back at home with Mom and Dad. Ultimately, we were able to get her on Medicaid. As we mentioned during the Symposium, that meant changes to providers, wait times to see providers stretching out from weeks to months, and Kalind’s health—mental and physical—declining. Many people know Angel by the moniker “Mama Bear” and she proved formidable in her data gathering and research skills and found the Diamond Headache Clinic in Chicago.
Angel was also a master at coping and distraction techniques. Consider this one: on the nine-hour drive to Chicago, one of the only things that kept Kalind occupied was pulling Kleenex one at a time from the box. Picture if you will Angel capturing each Kleenex as it floated through the cab of the truck as Kalind released it to be inserted into another box for Kalind to disassemble once she was finished with the current box. Nine hours of this activity. Mama Bear indeed!
The Diamond Headache Clinic proved to be lifesaving for the Perry family. The comprehensive integrative pain management offered there helped Kalind regain her health, her dignity and her independence—just in time to reverse roles and serve as caretaker in chief for her mom, Angel, when she was diagnosed with two kinds of aggressive cancer.
Kalind’s treatment continued once she returned home, with additional therapies outlined in our list above as she was able to access them. Insurance, access, and payment issues remained. When Kalind was once again able to work, getting time off from work to continue treatment became another issue. But it seemed that life was slowly getting back to a new kind of normal, albeit a normal that included life changed by a traumatic brain injury—some days were good, other days not so much. But that’s how it is for everyone, brain injury or not, right?
Then, early in 2020, Kalind was involved in what many would consider a minor fender bender in good weather on a busy highway on her way to work. No one went to the hospital, no tickets were issued, but with her history of brain injury, ANY bumps, jostles or jerks can set off the cycle and it takes longer to recover from each episode. Because the accident set off this new spiral, her employer didn’t understand and let her go. Employers don’t understand. They need employees to be present, but Kalind had not been at the job long enough to qualify for FMLA, plus this was a small company.
Once again, Kalind was experiencing crisis headaches, unable to work, some days unable to function, and she found herself back home with Mom and Dad. Two steps forward, three steps backward. No insurance, no income, no CIPM. Once again, we are grateful for family support, knowing that many don’t have that, but where is the social contract? Where do others turn for help? Where do we turn for help now other than one another?
Just as Kalind seemed to be turning the corner to brighter days, in 2016 Angel found herself shrouded in the dark clouds of cancer. Comprehensive integrative care proved much easier for Angel, however, because of the C word. All kinds of services were available not only to Angel, but to her family as well. Here’s where the WOW comes in!
- Massage therapy? You got it!
- Family support services? They’re yours!
- Physical therapy? Of course!
- Nutrition counseling? That’s so important; of course, we provide that!
All those services proved so helpful to Angel’s recovery, along with talk therapy, CBD products, vitamins, supplements and teas, along with meditation, long walks, and navigation services. Many of the services were covered by insurance, and we were indeed wowed by the coordination of care.
But now we’re in 2020, COVID-19 is a reality, and Angel faces a possible recurrence. Her immune system is shot, her family resources are limited, and Kalind’s resources are non-existent. Both Angel and Kalind require months of coordinated comprehensive integrative care.
So, what are our tasks going forward? What do we think YOU, as stakeholders in this quest, can do to help find that princess, give this movement sustained momentum?
Keep talking
Talk to family, friends, neighbors and most importantly, healthcare providers.
Few people truly understand what it’s like to live 24/7 with chronic pain.
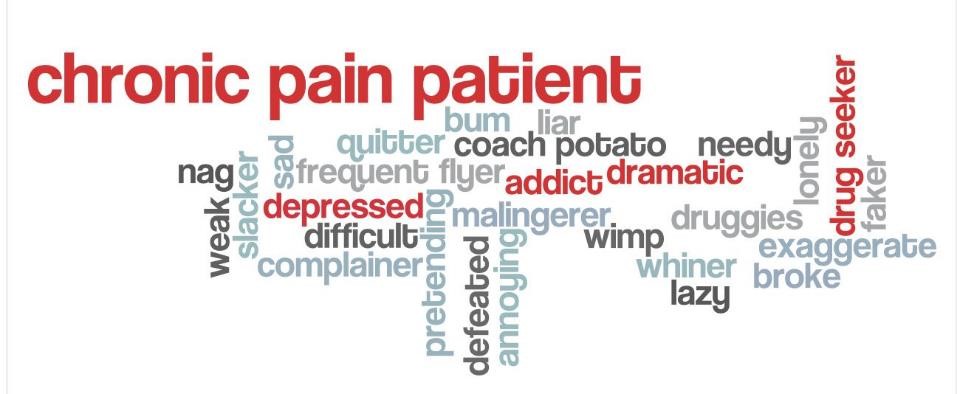
Help others understand that chronic pain does not equal opioid addition; it does not mean that you’re lazy, that you’re just depressed or difficult, that you’re not being dramatic. Instead, you live with a real disease, a disease that has rewired your brain. Education goes a long way towards helping others understand and moving to the new, correct narrative about those who persist and thrive with pain.
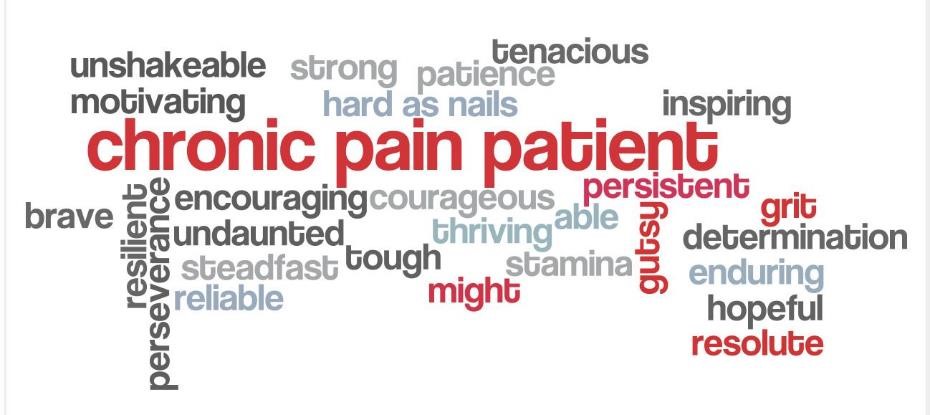
All too often, we think our healthcare providers should somehow intuit what we want and need. They are not mind readers. TELL them what you are experiencing. Communicate with them. Expect them to communicate with you. Don’t accept one-way conversations. Don’t accept the provider looking only at the computer. If that means you must find a new provider, then do that. YOU are the person living with pain. YOU are steadfast, reliable, tough and mighty.
If you’re working, talk with your Employee Benefits Coordinator and learn about the various benefits available to you. Is FMLA right for your circumstances? Would referral to the Employee Assistance Program be helpful? Are there accommodations that can be made to help you do your work? Develop a plan, including talking points, that show you as an asset valuable to the organization even with certain accommodations. It is important to present solutions—not just complaints—and to live up to those solutions.
Learn to advocate for yourself and others
Advocacy takes many shapes and forms. It’s about listening and discussing points of view with others in a non-judgmental manner, which can be very difficult when you know you’re being judged as a drug seeker. Persistence is key, however, in gaining services and the practical support we need to find our princess.
Myriad resources are available to learn how to advocate, including The Pain Community. Another good resource is The Community Tool Box, a public service developed and managed by the University of Kansas Center for Community Health and Development. Universities and libraries often have courses and/or speakers who can help identify resources for groups.
Learn to communicate YOUR story and put those advocacy skills to use where you are most comfortable. Some people find one-on-one advocacy most effective, while others revel in the legislative spotlight. Find your place to shine, find a mentor, and go for it. You don’t have to be an expert in public speaking. You are an expert in your lived experience with pain, and that’s what is important.
Providers, offer accessible hours and telehealth
When people who live with pain are fortunate enough to hold jobs, it’s very difficult to get away for appointments. If providers would offer hours other than the typical 8:00 am to 5:00 pm, we could more easily take advantage of them without jeopardizing our employment. COVID-19 has shown us that telehealth works; hopefully, that will continue past the pandemic.
Policymakers, consider a review of Workers’ Compensation
While Kalind’s experience may be unique, our non-scientific review of the evidence (talking with others) reveals differently. The benefits she received through Workers’ Compensation were minimal and fraught with difficulties, including disbelief and questioning of her integrity. It felt to us that the protection of the employer was paramount, rather than protection of the employee. Remember, though, that I (Angel) am Mama Bear! All joking aside, however, if we are striving for person-centered care, then our policies need to reflect that, and everyone should be worthy of respect.
So, how to conclude this quest for the elusive princess? We will keep doing what we know works for us—participating in PAINS-KC, visiting our different providers as possible, engaging in as many CIPM modalities as our budgets allow, and advocating on behalf of ourselves and others. We know that the repeating cycle for Kalind of pain, unemployment, and medical bills may be a reality, AND we know that the princess may very well be out there in the rain somewhere.
We’ll keep searching and put that pea in a museum when we find her. Will you keep helping us?

Trackbacks/Pingbacks