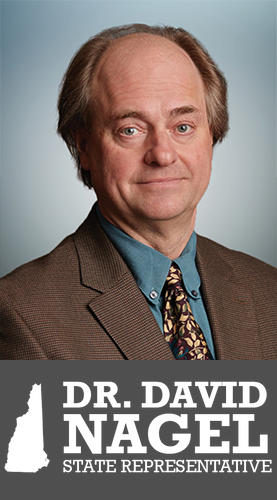
 Recently, AACIPM Director Amy Goldstein sat down with David Nagel, MD, to catch up on all the exciting work in his world. Dr. Nagel, who is dual-board certified in Physical Medicine & Rehabilitation and Pain Medicine, is thrilled to see the recently-released Pain Management Guide for the NFL PA (National Football League Players Association) after years of his hard work and leadership co-chairing the committee. Further, huge congratulations are in order, as Dr. Nagel ran for office and was elected on November 8 to represent Belknap 6 in the New Hampshire House of Representatives.
Recently, AACIPM Director Amy Goldstein sat down with David Nagel, MD, to catch up on all the exciting work in his world. Dr. Nagel, who is dual-board certified in Physical Medicine & Rehabilitation and Pain Medicine, is thrilled to see the recently-released Pain Management Guide for the NFL PA (National Football League Players Association) after years of his hard work and leadership co-chairing the committee. Further, huge congratulations are in order, as Dr. Nagel ran for office and was elected on November 8 to represent Belknap 6 in the New Hampshire House of Representatives.
AACIPM: Dr. Nagel, you have been in practice for decades, working to help people with pain live better lives. What are your biggest opportunities and challenges right now?
Dr. Nagel:
I think, unfortunately, we still have more challenges than opportunities.
The opioid crisis really had a dramatic, adverse effect on pain care in our country. It was hard to take such a step back; yet still, there is an opportunity. I have worked to create community based, integrative pain care since I started my practice, and I have worked on pain care policy and opioid policy in our state for nearly 30 years. I was really proud of what we accomplished, but I am concerned that when all we pay for is pills and procedures, that is what we get. There is little evidence to suggest that so-called interventions and opioids, by themselves, have any cost-benefit for our patients. I don’t believe in magic bullets, and I am convinced we are putting too many dollars in these treatments and that needs to change. I really believe we need to spread the wealth among all therapeutic options, allopathic and non-allopathic (complementary/alternative), and do so in an integrative, patient centered, communicative way. I am working hard in our state to see that happens, and I really believe the opioid crisis has given us the means to accomplish this.
With that said, we are finding some adversaries in this endeavor. There are some providers who are resistant to change due to payment structures, and there are also payers who are reluctant to open up new cost streams, even though they could finance it by diverting money from expensive interventions that don’t work to substantially less expensive integrative care that does work. That said, we are also creating networks of friends. When we last testified before our legislature on increasing access to care, it was really neat to see the broad array of stakeholders speaking with one voice. Collaboration makes this fun and worthwhile.
AACIPM: How did you get involved with NFL PA, and what is important for us to understand about the Pain Management Guide that has been released? We love the opening paragraph here which is: “The best approach to treating pain is choosing a combination of options provided by pros who collaborate on your care. Evaluate the risks and benefits of treatments and create a personal plan to maximize your performance through effective pain management.”
Dr. Nagel:
After tackling the issue with CTE [chronic traumatic encephalopathy, a concussion-related brain disease], the NFL PA wanted to take on pain care in players. They reached out to the pain community to find “experts.” Myra Christopher was asked, and I was honored that she recommended me, based on our interactions together, and on my book, Needless Suffering, How Society Fails Those with Chronic Pain. The NFL PA looks at this as a labor-management issue, and Betsy Gilbertson, who the guide is named for, and I both have strong labor-management backgrounds.
I was excited about this opportunity for several reasons. First, my first experience in advocacy was with post-concussive syndrome. When the NFL PA took this issue on, I was amazed by how much easier my work became, as I was able to win cases in court merely by citing the NFL. I thought that this could work similarly for pain care. Second, I had a vision of creating a consumer-oriented, evidence-based, pain care guide that would empower athletes, active and retired, with the knowledge they needed to manage their own care, and then use this model to trickle down to the general public. In order to do this, I interviewed athletes at all levels of participation, from pee-wee to elite. I was shocked to find out how little they trusted the medical staffs involved in their pain-care. Sound familiar? It became quite apparent there was a need for such a guide.
Because I had a vision for this pain care guide, I was asked to co-chair the endeavor. It took five long years, but it is finally out and available to the public. The PDF version is available, and that is the better version to review. Throughout the process, I insisted this be available to the public, as I believe, based on the CTE experience, that NFL PA has the power to change social policy for the greater good—and I really hope we have made a good start on this. This was designed to be a living document, one easy to adapt, and thus would be very helpful to have feedback.
I wrote most of the introduction section to the guide and several of the modality sections. It was important to me that we stress empowerment, integrative care, patient centered care, whole-life/whole person care, and family involvement. All these were stressed, as you say in your question. We stressed modalities in order of importance, and we listed physical restorative and complementary modalities first. Interventional and surgical modalities were far down the list. The weakness of other best practice guides was the lip service they pay to these modalities and how they greatly over-emphasize the value of pills and procedures. We worked hard to fix that deficiency.
Also, importantly, our focus was on acute pain and what we have come to call “acute pain chronically,” both of which are issues for athletes. However, I believe the guide generalizes to those with chronic pain. I also believe this idea of “acute pain chronically” is an entity that we really need to explore. It is a lot more common than we are led to believe, and will change the way we look at chronic pain.
AACIPM: In your clinical work, you seek out relationships with other providers to create the best care for your patients. An example is your work with acupuncture. Has this made a difference in the lives of your patients?
Dr. Nagel:
Most definitely. I think of the house of pain management Biblically, as a place with many rooms and a place for all providers. The whole is greater than the sum of the individual parts, especially when we work together. My practice of acupuncture opened up whole new ways of thinking about bio-psycho-social-spiritual health and wellness and also introduced me to a whole new world of talented and thoughtful providers I could learn from.
What I am concerned with, though, is that in expanding the “medical-industrial complex”, we have created artificial barriers between providers in our communities that often impairs collaboration and communication and stigmatizes those with complex medical problems. These barriers were not like that when I started my career, and they really need to change.
AACIPM: Clearly, grass does not grow under your feet, as we have always known. You recently ran for state representative and have won a seat representing your district in the New Hampshire House of Representatives. Congratulations! What led you to the decision to run?
Dr. Nagel:
I did win my election. Yippee! Now the work starts.
Years ago, my mom, who is my hero, was functionally bullied by an able-bodied person who verbally pushed her out of the way. My Mom had severe rheumatoid arthritis and was very limited. I was so angered by this stigmatization that I felt a need to stand up for her and others like her. My mom always stood up for those in need. She couldn’t walk well, but she had a finger and a phone and she created a model of what I call kitchen-table advocacy. The world did not treat her well, but she did her best to not let that happen to others. She has always been my inspiration. I joke that I am a middle child born on a Wednesday; I get in the middle of everything. I have always felt a need to stand up for the marginalized. I am amazed at the power of the letters “MD” that allow me to do that, both in my practice and in the broader social realm.
I chose to run because I believe that I can have greater power to make social change as in insider than an outsider. I fully accept that may be an illusion, but one I feel compelled to follow. My priorities are to eliminate barriers to health care for those disparaged: those in pain, those suffering from mental health problems, those with addiction, those of color or other ethnicities, women, veterans, children, etc. I am very interested in Native American rights in our state. We are trying to create a world of inclusion.
AACIPM: Not everyone is as comfortable engaging in policy and advocacy activities as you are. Any thoughts or advice for the range of stakeholders that are involved with AACIPM who may want a nudge to get more involved?
Dr. Nagel:
I learned a long time ago, if you are not involved, they won’t hear you. It is very easy to whine about how things are, but whining accomplishes nothing. I also learned how hard decision making gets in the political arena, and, dare I say, I have developed a respect for those who struggle to make fair decisions. I have created a primer for advocacy that you may have inspired me to publish. There all sorts of ways of getting involved. My Mom used the phone. My model is what I call John the Baptist advocacy: a voice crying in the wilderness. You need to find a model that suits who you are. Never try to be someone you are not. Mother Teresa understood this intuitively—in her Mission, she found a place for everyone who had a desire to help, no matter what their physical, spiritual, intellectual, or social limitations may be.
AACIPM: AACIPM focuses on connecting the dots to advance access to quality, person-centered pain care. You have connected the dots in your own area. What else do you have to say about the importance of collaboration and finding ways to work together?
Dr. Nagel:
As Bob Twillman is fond of quoting Mencken and Twain: “For every complex social problem, there is a solution that is neat, simple, and wrong.”
I have always been more intrigued by the complex. I have long been amused by the fallacy of simple solutions. When I began studying the problem of pain, first intuitively as a child, later as a professional, I searched all over for wisdom, and found wisdom comes from all places. I have always said I learn more from my patients than I do from my professors. The worst thing you can ever do is close your mind to the thoughts of others. Collaboration opens your mind and helps you solve problems you never would otherwise. I really believe that most of the self-inflicted problems in our world have come from a failure to be willing to collaborate. In running for office, I chose to run as a Republican. I was endorsed by two Democratic party groups and by two labor unions. I would like to think that the reason is because I value ideas more than the letters “D” and “R.” I would also like to believe our world is hungry for such an approach to problem solving, and I really hope this is part of a multi-colored wave that will sweep our country, our world, and find ways to help those in need.