Symposium

AACIPM was honored to participate in the International Congress on Integrative Medicine and Health 2022, held in Phoenix, Arizona, May 23-26. This Congress was convened by the Academic Consortium for Integrative Medicine and Health.
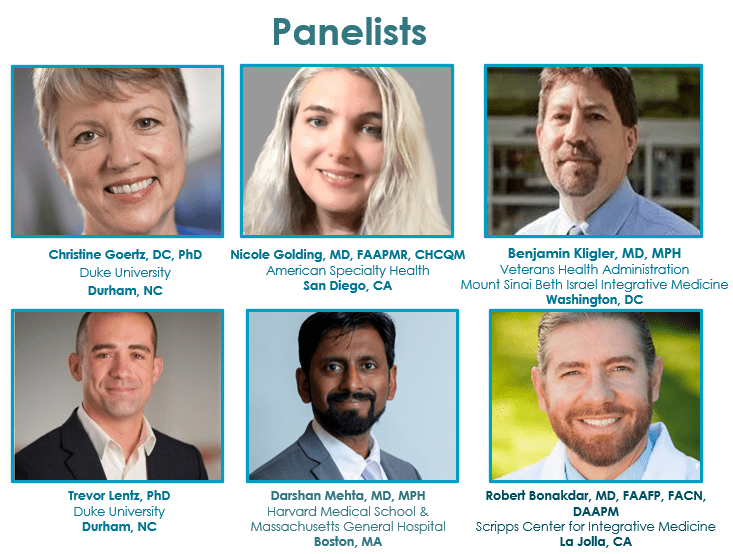
Historically, more than 1,000 researchers, educators, clinicians and trainees from around the world attend. Robert Bonakdar, MD, FAAFP, FACN, Director of Pain Management, Scripps Center for Integrative Medicine and Amy Goldstein, MSW, Director, AACIPM, organized this session along with fabulous panelists:
A Multi-Stakeholder Discussion about Overcoming Obstacles on the Path to Comprehensive Integrative Pain Management
A synthesis of public health challenges, from the ongoing drug overdose epidemic to high health care costs and overuse, have driven significant interest in advancing whole person models of care for pain. In light of evolving science and medicine, authorities across the United States recommend that providers of pain care should treat patients with an approach that is comprehensive, integrative, multi-disciplinary, multi-modal, and, most importantly, individualized and person-centered. However, delivery of comprehensive patient-centered pain care is a multi-sector issue that requires adequate data, evidence, and collaboration across sectors to establish the most practical ways to deliver and pay for that level of care.
The majority of current clinical guidance, including recommendations published by prominent organizations such as the American College of Physicians and the Veterans Health Administration, encourages use of integrative treatment modalities as part of comprehensive pain care. But despite growing evidence supporting these therapies, universal expansion and implementation of recommendations remains limited. Substantial resources are being spent to address key obstacles related to access, education, perception and coordination that hinder widespread dissemination and uptake of comprehensive integrative pain management (CIPM). Simultaneously, a number of research and state initiatives have approached these barriers with innovative solutions. This session will review the current rationale supporting an integrative model of pain care, and discuss critical information and evidence gaps that must be addressed to support greater implementation of CIPM. We will identify potential action steps to increase integration of complementary and integrative approaches for the millions of people in need of quality pain care.
Co-Moderators
References and Resources
- Duke Margolis Ortho Case Study: Exemplary Integrated Pain Management Programs: West Virginia University Center for Integrative Pain Management (WVUCIPM), Katie Huber, MPH, Jonathan Gonzalez-Smith, MPAff, Robert Saunders, PhD, Christine Goertz, DC, PhD, Trevor A. Lentz, PT, PhD, MPH
- Duke Margolis Ortho Case Study: Exemplary Integrated Pain Management Programs: University of Vermont Medical Center Comprehensive Pain Program, Jonathan Gonzalez-Smith, MPAff, Katie Huber, MPH, Robert Saunders, PhD, Christine Goertz, DC, PhD, Trevor A. Lentz, PT, PhD, MPH
- Duke Margolis Ortho Case Study: Exemplary Integrated Pain Management Programs: People’s Community Clinic Integrative Pain Management Program (PCC IPMP), Katie Huber, MPH, Jonathan Gonzalez-Smith, MPAff, William Bleser, PhD, MSPH, Robert Saunders, PhD, Christine Goertz, DC, PhD, Trevor A. Lentz, PT, PhD, MPH
- Duke Margolis Ortho Case Study: Exemplary Integrated Pain Management Programs: University of New Mexico Pain Consultation and Treatment Center (UNM Pain Center), Katie Huber, MPH, Jonathan Gonzalez-Smith, MPAff, Robert Saunders, PhD, Christine Goertz, DC, PhD, Trevor A. Lentz, PT, PhD, MPH
- Gallup MD Recommendations: Patient-Reported Physician Treatment Recommendations and Compliance Among U.S. Adults with Low Back Pain, Christine M. Goertz, DC, PhD, Cynthia R. Long, PhD, Cynthia English, MPP, William C. Meeker, DC, MPH, and Dennis M. Marchiori, DC, PhD
- Health Services Research – 2022 – Bokhour: From patient outcomes to system change: Evaluating the impact of VHA’s implementation of the Whole Health System of Care, Barbara G. Bokhour PhD, Justeen Hyde PhD, Benjamin Kligler MD, MPH, Hannah Gelman PhD, Lauren Gaj BA, Anna M. Barker MS, Jamie Douglas MA, Rian DeFaccio MS, Stephanie L. Taylor PhD, Steven B. Zeliadt PhD
- IPM NEJM Catalyst 2020: Managing Multiple Irons in the Fire: Continuing to Address the Opioid Crisis and Improve Pain Management during a Public Health Emergency, Trevor Lentz, Christine Goertz, Isha Shama, Jonathan Gonzalez-Smith, Robert Saunders
- J. Bjornaraa Cognitive Behavioral Coaching Program with Low Back Pain: Effects of a Remotely Delivered Cognitive Behavioral Coaching Program on the Self-Rated Functional Disability of Participants with Low Back Pain, Jaynie Bjornaraa, PhD, MPH, PT, Anne Bowers, PhD, David Mino, MD, MBA, Denee Choice, MD, PT, Douglas Metz, DC, Kimberly Wagner, RN
- Legoretta Archives Utilization: Comparative Analysis of Individuals With and Without Chiropractic Coverage: Patient Characteristics, Utilization, and Costs, Antonio P. Legorreta, MD, MPH; R. Douglas Metz, DC; Craig F. Nelson, DC, MS; Saurabh Ray, PhD; Helen Oster Chernicoff, MD, MSHS; Nicholas A. DiNubile, MD
- Management of Low Back Pain: Initial Management of Acute and Chronic Low Back Pain: Responses from Brief Interviews of Primary Care Providers, Eric J. Roseen, DC, MSc, Frank Garrett Conyers, MD, MPP, Steven J. Atlas, MD, MPH, and Darshan H. Mehta, MD, MPH
- Metz JOEM Substituion Care: Chiropractic Care: Is It Substitution Care or Add-on Care in Corporate Medical Plans? R. Douglas Metz, DC, Craig F. Nelson, DC, MS, Thomas LaBrot, DC, Kenneth R. Pelletier, PhD, MD(hc)
- NAS NonPharm Workshop Proceedings: National Academies of Sciences, Engineering, and Medicine 2019. The Role of
Nonpharmacological Approaches to Pain Management: Proceedings of a Workshop.
Washington, DC: The National Academies Press. https://doi.org/10.17226/25406. - Nelson JMPT Procedures: Effects of a Managed Chiropractic Benefit on the Use of Specific Diagnostic and Therapeutic Procedures in the Treatment of Low Back and Neck Pain, Craig F. Nelson, DC, MS, R. Douglas Metz, DC, and Thomas LaBrot, DC
- Stress Landscapes: Identifying Stress Landscapes in Boston Neighborhoods, F. Garrett Conyersm, MD, MPP, Helene M Langevin, MD,
Gary J Badger, MS, and Darshan H Mehta, MD, MPH - Invited Commentary LWW Medical Care: The Whole Health Transformation at the Veterans Health Administration: Moving From “What’s the Matter With You?” to “What Matters to You?” Benjamin Kligler, MD, MPH, Justeen Hyde, PhD, Cynthia Gantt, PhD, FNP-BC, FAANP, and Barbara Bokhour, PhD
- AAMC Journal of Teaching and Learning Resources Article: Implementing an Interactive Introduction to Complementary Medicine for Chronic Pain Management Into the Medical School Curriculum, Uttara Gadde, Pravin Matthew, Raagni Kumar, Rashi Aggarwal, MD, Michelle Dalla Piazza, MD, Sangeeta Lamba, MD, MSHPE
- BMC Family Practice Research Article: Barriers and facilitators to use of non-pharmacological treatments in chronic pain, William C. Becker, Lindsey Dorflinger, Sara N. Edmond, Leila Islam, Alicia A. Heapy, and Liana Fraenkel
- Journal of Pain Management Nursing Article: How Patient Education Influences Utilization of Nonpharmacological Modalities for Persistent Pain Management: An Integrative Review, Iquo N. Andrews-Cooper, DNP, APRN, FNP-C, Sharon L. Kozachik, PhD, RN, FAAN
- Research Report: Medical Trainees’ Experiences of Treating People With Chronic Pain: A Lost Opportunity for Medical Education Kathleen Rice, PhD, Jae Eun Ryu, Cynthia Whitehead, MD, PhD, Joel Katz, PhD, and Fiona Webster, PhD
- Journal of Pain Research Article: Using social media to challenge unwarranted clinical variation in the treatment of chronic noncancer pain: the “Brainman” story, Ruth White, Chris Hayes, Scott White, Fiona J Hodson
Panelist Bios
Robert Alan Bonakdar M.D., FAAFP, FACN
Dr. Bonakdar is a 2018 Mayday Pain Fellow and the Director of Pain Management at the Scripps Center for Integrative Medicine since 2002 and a member of the systemwide Opioid Stewardship Committee. He is theco-editor of the Oxford University Press textbook of Integrative Pain Management. Most recently, Dr. Bonakdar has presented to the congressionally mandated Pain Management Best Practices Inter-AgencyTask Force as well as at The National Academies of Sciences, Engineering, and Medicine on non-pharmacological approaches to pain. Prior to medical school, Dr. Bonakdar received a Richter International Fellowship where he studied Eastern healthcare approaches in Southeast Asia. After completing his medical training, he completed a fellowship at the Scripps Center for Integrative Medicine/ Scripps Clinic with a focus on integrative pain management. Additionally, he is certified in headache management by the United Council for Neurologic Subspecialties and board certified in Integrative Medicine by the American Board of Integrative Medicine. Dr. Bonakdar has a special interest in nutrition and the is founder and course director of the Scripps CME conference Natural Supplements: An Evidence-Based Update, now in its 18th year. He is also a fellow of the American College of Nutrition and recipient of the 2020 ANA Mark Bieber Award.
Christine Goertz
Christine Goertz, D.C., Ph.D. is a Professor in Musculoskeletal Research at the Duke Clinical Research Institute and Director of System Development and Coordination for Spine Health in the Department of Orthopaedic Surgery at Duke University. Dr. Goertz’s 25-year research career has focused on working with multi-disciplinary teams to design and implement clinical and health services research studies to increase knowledge regarding the effectiveness and cost of complementary and integrative healthcare delivery. She has received nearly $32M in federal funding and has authored nearly 100 peer-reviewed papers. Dr. Goertz was appointed and is currently Chairperson of the PCORI Board of Governors.
Nicole Golding
As Medical Director of Health Services at American Specialty Health, a complementary healthcare and fitness benefits management company, Dr. Golding, MD, FAAPMR, CHCQM, is involved with evidence evaluation/ policy development, utilization management, professional affairs, accreditation activities, quality of clinical/ health/ fitness programs, development/incorporation of cognitive behavioral coaching into MSK pain management health plan programs, and supports sales clinically with potential health plan clients. Dr. Golding has worked at the CDC, The Carter Presidential Center, attended Emory and Mercer Universities, trained at Columbia and Cornell, then in China for acupuncture, and is Board Certified in Physical Medicine and Rehabilitation, as well as Health Care Quality and Management. She practiced Rehab Medicine for over 20 years in both outpatient integrative pain management and inpatient rehabilitation settings, prior to joining ASH 5 years ago.
Amy Goldstein
Amy Goldstein, MSW, has been in the healthcare field for 25 years, advocating for the needs of people and families. Amy is driven to promote effective advocacy work by identifying unique combinations of stakeholders who share interests and a desire to change the current health paradigm. She developed and currently directs the grant-funded initiative Alliance to Advance Comprehensive Integrative Pain Management after previous roles at the Academy of Integrative Pain Management, National Multiple Sclerosis Society and American Cancer Society. Amy is committed to strategic thinking and finding meaningful ways to improve access to whole person, quality pain care for all.
Benjamin Kligler
Benjamin Kligler is the Executive Director of the Office of Patient Centered Care & Cultural Transformation at the Veterans Health Administration, United States Department of Veterans Affairs. He is also the immediate past chair of the Academic Consortium for Integrative Medicine and Health and an associate Professor of Family Medicine at Icahn Mount Sinai School of Medicine.
Trevor Lentz
Trevor A. Lentz, PT, PhD, MPH is an Assistant Professor in Department of Orthopaedic Surgery at Duke University School of Medicine and a member of the Duke Clinical Research Institute. His clinical research interest in individual and health care system-level factors that influence patient-reported outcomes, opioid use, health care utilization, and costs following orthopedic injury and surgery. He focuses on improving care for people with musculoskeletal pain by 1) developing tools to evaluate psychological distress and behavioral needs in clinical practice, 2) re-designing care models to account for multi-morbidity, and 3) identifying and addressing health system barriers to high-value care.
Darshan Mehta
Medical Director and Director of Medical Education for Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital (BHI-MGH) and Director of Education at Osher Center for Integrative Medicine, Harvard Medical School and Brigham and Women’s Hospital (OCIM). Educational and research interests include curricular development in complementary/integrative medical therapies, mind/body educational interventions in health professions training, and promotion of professionalism in medical trainees. Directs medical student/resident rotational electives at BHI-MGH and Osher Center. Provides a consultative role with patients at both locations. He serves on Education and Membership Committees for the Consortium of Academic Health Centers for Integrative Medicine (CAHCIM).



