CIPM Practice Examples
AACIPM’s Repository of Clinical Practice Examples
Innovation and Progress
This repository illustrates innovation and progress in current clinical practice examples towards equitable, whole person centered, multi-modal pain management. This is designed to be of interest across the stakeholders – including people with pain, providers, insurers, purchasers, researchers and more. We aim to connect the dots to advance CIPM business models that practices can adopt, and payers and purchasers can recognize as clinical practices that are worthy of coverage.
Op-Ed
Opinion piece about why this is important
AMA’s Story: Putting the “Multi” in Multimodal Care for Patients with Pain
An example of integrative pain care from American Medical Association AACIPM thanks one of our many collaborators, International Association of Yoga Therapists (IAYT), who introduced us to Inner Atlas, a unique method of facilitating whole person, multimodal pain care...
Duke Releases Two Case Studies on Person-Centered Integrated Pain Care
Both ‘exemplary’ pain programs focus on improving access to care in medically underserved communities and integrating with primary care The Duke-Margolis Center for Health Policy and Duke Orthopaedic Surgery are announcing the release of two exciting new studies on...
Duke Releases Case Study on Comprehensive Pain Program Using Unique Bundled Payment Arrangement
AACIPM is pleased to share that the Duke-Margolis Center for Health Policy and the Duke Department of Orthopaedic Surgery have released the second of four case studies emanating from their 2020-21 Roundtable on Integrated Pain Management. Their second case study...
AMA’s story Texas FQHC Develops Integrative Model for People with Pain | Advocacy Efforts to Improve Access
New story in American Medical Association’s microsite, End the Epidemic People with acute and chronic pain, especially those who are underserved, face significant challenges accessing person-centered, multidisciplinary, comprehensive integrative pain management. This...
Spotlight: Dr. Joanna Katzman on ECHO
An interview with Joanna G. Katzman, MD, MSPH, Professor, UNM School of Medicine; Director, UNM Pain Center; Director, ECHO Institute, Pain, Substance Use and Public Health Programs Please provide a brief history and description of the University of New Mexico Pain...
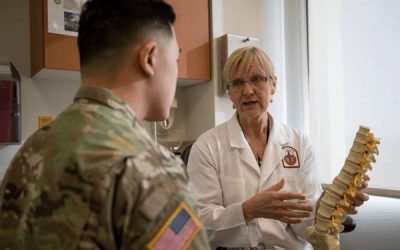
The Connector: Spotlight – Madigan Interdisciplinary Pain Management Centers
An interview with Diane Flynn, MD, primary care physician at Madigan's Interdisciplinary Pain Management Center The Interdisciplinary Pain Management Centers (IPMC) at Madigan and at other Army Medical Centers were established in 2010 at the direction of the Army...
AMA’s Story about WVU Comprehensive Integrative Pain Management in Action
You may have seen this excellent panel discussion during AACIPM's May Symposium with Dr. Clay Marsh, Dr. Rick Vaglienti, and Julianne Speeney about the transformation at West Virginia University Medicine Center for Integrative Pain Management to approach pain in a...
Guest Spotlight: Sharad Kohli
Access to Comprehensive Integrative Pain Management for People in the Safety Net An interview with Sharad Kohli, MD You work at People’s Community Clinic – what kind of a clinic is this? People’s Community Clinic (PCC) is a Federally Qualified Health Center (FQHC)...
Related Resources
Related Article:
National Governors Association, Expanding Access to Non-Opioid Pain Management
See AACIPM Webinar about Equity in Access to Comprehensive Pain Management
Related Article:
Agency for Healthcare Research & Quality, Integrated and Comprehensive Pain Management Programs, Effectiveness and Harms
See AACIPM Letter to AHRQ concerning this Request for Information
Advancements in Comprehensive Integrative Pain Education
Sign up to receive our updates
Sign up to receive our updates